A midwife in North Carolina was recently charged with practicing midwifery without a license because her state does not offer licensure for Certified Professional Midwives (CPMs) and other direct entry midwives. There was some local news coverage of the arrest and the ongoing efforts of North Carolina families to legalize CPMs. One of the local news stories included a mother’s birth story from the “If I were at home, I would have died” perspective.
When I hear statements like this I cringe on the inside. Being a midwife, I hear it a lot. Women love to talk about their birth stories, as they should; Storytelling is a natural and beautiful part of our collective journey as women and mothers. In the park, at mom’s groups, among new friends, anywhere women gather there are stories of births and babies being told. When I hear a story being told from the “I would have died at home” perspective, I do my best to nod with genuine empathy. I want to support each woman’s telling of her own story. BUT, it’s a bit of a double bind (midwives and doulas — you know what I am talking about).

A typical hospital birth hook-up: pitocin to speed up labor, epidural medication, and an IV bag. Pitocin use in labor makes women more likely to hemorrhage after birth.
In these moments, I strive to listen with an open heart, gentleness and love. Every woman’s story is inherently valid and it is her story to tell, her journey. The reality however is that these emergencies women experience are very often caused by unnecessary interventions in their labor or birth. A huge part of my journey in birth work has been to advocate for truth and justice in maternity care and to illuminate the myths and realities of the hospital birth industry. The best I can do in these situations is honor the mother’s feelings and experiences while side-stepping all the nuts and bolts of the “I/we would have died” argument.
Since a larger audience of women is hearing such emotionally charged statements about homebirth in the media feeding frenzy lately, let’s take a closer look. Why do women in the US die while giving birth? No one knows for certain because our reporting methods for maternal mortality are so abysmal. We think, based on fractured US statistics and older studies, that the primary causes of death to women during birth or shortly after are thromboembolism, preeclampsia/eclampsia, hemorrhage, infection, and anesthesia deaths.
Lets look at hemorrhage because it is the most likely of these unlikely complications to occur in low-risk women birthing at home. Here are a few reasons why. Homebirth and hospital birth are supported by two divergent models of care. The homebirth model subscribes to the philosophy of don’t fix what isn’t broken: natural processes generally work best when they are not interfered with. The medical model subscribes to the (more profitable) philosophy of action: pregnancy and birth are conditions that require fixing. All actions and interventions have consequences. Many of the interventions in a typical hospital birth cause complications, like hemorrhage. These interventions are far less likely to occur during homebirths attended by midwives.
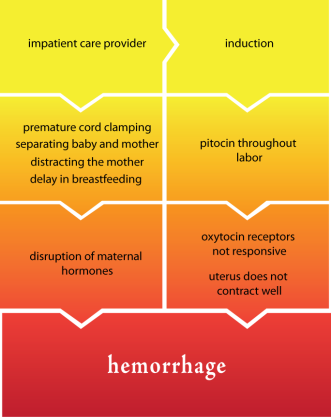 New research demonstrates that women whose labors are altered by prolonged exposure to pitocin are more likely to hemorrhage after their birth. This is because oxytocin, our body’s own version of pitocin, helps the uterus to contract after birth and minimize blood loss. Pitocin binds to oxytocin receptor sites, and over time the body becomes desensitized to it, preventing the uterus from contracting normally and leading to hemorrhage. Regrettably, we’ve gotten to a point now where most births in the US are started artificially with the help of pitocin (induction) or hurried along by it (augmentation). Homebirth midwives do not use pitocin to start or speed up labor.
New research demonstrates that women whose labors are altered by prolonged exposure to pitocin are more likely to hemorrhage after their birth. This is because oxytocin, our body’s own version of pitocin, helps the uterus to contract after birth and minimize blood loss. Pitocin binds to oxytocin receptor sites, and over time the body becomes desensitized to it, preventing the uterus from contracting normally and leading to hemorrhage. Regrettably, we’ve gotten to a point now where most births in the US are started artificially with the help of pitocin (induction) or hurried along by it (augmentation). Homebirth midwives do not use pitocin to start or speed up labor.
Immediate postpartum interventions can also lead to hemorrhage. The period just after birth is a unique and potent time biologically for the mother and baby. A natural flood of hormones connects mother and baby physically and emotionally, and helps the mother safely birth her placenta. The mother’s hormone levels will never be as high as this hour after birth; and when this flow is disrupted the mother is more likely to bleed excessively.
Interventions during this immediate postpartum time are routine in a hospital setting: failing to give the baby to the mother immediately, assessing the baby away from the mother, pulling on the umbilical cord, changing the mother’s position to suit the care provider, diverting the mother’s attention away from the baby, clamping and cutting the umbilical cord without any good reason to do so, etc.
Midwives honor the biological importance of the hormonal bubble after birth and do not intervene unless the mother or baby needs help.

In a typical homebirth, mother and baby are undisturbed after birth. The midwife does not unnecessarily poke, prod, clamp, or otherwise interfere with the mother and baby unit.
When you hear someone say “I would have died if I had a homebirth” or “my baby would have died,” please remember that these are very emotionally charged declarations. And yes, they may be true statements. Yet tragic outcomes DO occur in any setting despite the “best” possible care — hospital or home. However, in many hospital births, it is unnecessary interventions that have caused the complications that women and babies suffer from. The CDC has estimated that half of maternal deaths are preventable.
You cannot simply cut and paste all the circumstances surrounding a given hospital birth, superimpose them on a homebirth setting, and predict the same outcome — or vice versa. The models of care are too divergent. Women can die from birth complications in any setting, and our hospital death rate from birth-related causes is indefensibly high. We know that low-risk women are as safe, if not safer, birthing at home.
The United States ranks 41st in maternal mortality among nations. That means in 40 other countries, women are less likely to die from pregnancy and birth related causes. The CDC also states that half of the reported deaths were preventable and that death rates are underreported by almost a third. On April 9th the Healthy Mothers Healthy Birth Summit will convene in Washington D.C. to examine the clinical and political issues surrounding maternal death in the United States.
Erin –
This is so beautifully and factually written. Thank you for shedding light on this very important topic. I was particularly moved by your comparison of the “don’t fix what isn’t broken” and “action” models and this sentence, ” You can’t simply cut and paste all the circumstances surrounding a given hospital birth, superimpose them on a homebirth setting, and predict the same outcome — or vice versa.” May we all remember the incredible power of natural processes and the individuality of each person, moment, and circumstance.
Please write more on this in the future…
Dr. Holcomb
Thank you Erin! Thank you so much!! I’m sure you won’t have any trouble recalling the fact that both Colin’s and my family gave us a very very hard time about our decision to give birth at home. Having something like this to show them and have them read will be so valuable when we hopefully get to do it again someday!!
Oh Melissa, when you do it again you will know in your heart and mind that you are making the best decision for yourself and your baby (whatever that decision is), and that is what matters. I know that it *feels* so much better though to have family on board. Once you experience family-centered birth at home you want everyone to see the power and love in non-institutionalized birth.
Good article.
I am one of the minority who did hemorrhage at home. It was no ones fault and my midwife did everything in her power and then called 911. She saved my life. Obviously this wasn’t the ideal circumstances but she has had midwife training and knew what to do. Midwives can do a lot in less than perfect situations, including calling for help if need be.
I had a beautiful homebirth and I wouldn’t have had it any other way just because there was a slight glitch. My second child was born out of hospital as well with no complications. 🙂
Thank you Lysa for sharing your story. I did not get into the midwifery management of hemorrhage at home because, well, that’s another (long) post! It is important for folks to know that although less common, hemorrhage can happen at home, and that it is typically quickly resolved with the help of a skilled midwife. In rare cases a mother may need the higher level care or ongoing monitoring a hospital provides, and we are blessed to have that resource.
Absolutely! I hemorrhaged with my fourth child (a UC) but I was one block from the hospital. It actually was dealt with faster than my second birth where I hemorrhaged so badly from them pulling my placenta out, that I had a seizure and went into shock. My 5th birth was midwife assisted and just as perfect as a homebirth could have been. I wish more people had the availability of trained midwives and cooperative hospitals if they do need to transfer care!
yes, with my HBA3C my midwife had a great back up plan in place. 🙂 (it made my hubby feel better!)
40 hours later baby girl was born… whew. lol
thank you for the post erin!
9 months goes by sooo fast…i sure wish for any to be mommas out there …PLEASE REMEMBER WOMEN ARE ….amazing OUR bodies do indeed have an amazing capacity to succeed and endure
I was an amazing low risk very healthy 36 first pregnancy….i watched Business of being Born..i so much wanted to birth at Middleton Birth Center …but $$ and my husband believes doctors know best… hospital birth it was…ugh i wasnt thrilled. I decided if that was the cards i was dealt then i was at least going to hire a doula to be my advocate.
We checked in at hopital @4cm…..lotsa pain in my rectum area….supposedly Baby O.. was sunny side up…my awesome doula suggested different positions and such..my doc kept wanting to check to see how dilated i was a couple of times i adamantly said NO!!… i mean seriously..i qm having contractions and you want to perform a finger insertion on my cervix? …ugh….i was i think in retrospect…very tense..and i know that i felt like i was wastinf everyones time…in retrospect if i could have just said to all nurses just leave me alone until i need you…ugh!!
Fast forward 12 hours..
Dr said hmm “youu are not progressing…you have only dilated 1cm in 10hrs”…and i clearly had lota pain in my rectum area with each contraction..and since i had no interest in really eating or drinking (thought it would make me poop everywhere if i ate…and i was trying to avoid the embarassmment of a potential situation by not eating..)…ughhh…
I REALLY WISH MY AWESOME DOULA WOULD HAVE PULLED ME ASIDE AMD SAID…”what you ate going thru with a slow progression is entirely normal…But BE AWARE THAT SINCE WE ARE IN A HOSPITAL…they are going to want to speed things along….i wish my doula would have said…YOU HAVE THE POWER TO SAY NO TO ANY INTERVENTIONS…YOU REALLY CAN DO THIS!!
ugggh… i seriously wish my doula could have painted the picture CLEARLY FOR ME..i wish she could have said…if i dont drink x amount in the next hour then they will make me take an IV..
I wasnt thinking clearly and i was
“You can’t simply cut and paste all the circumstances surrounding a given hospital birth, superimpose them on a homebirth setting, and predict the same outcome — or vice versa. The models of care are too divergent. ”
SUCH a good point!
I try to approach every birth I attend with the intention of doing nothing besides being a quiet presence for the mother and the bare minimum of interference being aware that even the most innocuous intervention (such as listening to heart tones) may break a mother’s concentration or cause her to change her patterns of behavior. In the hospital, there is little to no protection of the mother, she is at the mercy of the hospital routine. Most peopke fail to appreciate just how important it is to leave the mother undisturbed. They welcome the disturbance because they have been conditioned to believe that it is safer.
Very good, thought provoking post!
Yes Bettie! You raise an excellent point — everyone is busy protecting themselves in the hospital, there is no one to protect the mother.
I agree with your article and think home births are a great option for women in almost all cases. I do want to add though, being an L&D nurse on a very busy OB unit, that quite a few nurses (and sometimes even doctors) do actually work very hard to protect their patients and the experience that they desire. Just as a lot of people only hear about the home births that don’t go well, you often don’t hear about the beautiful natural, no intervention deliveries that happen everyday in hospital settings.
Deanna, I don’t disagree with you. I know many wonderful people who work hard on OB units to give great care to mothers. The point I was making is that undisturbed birth generally never happens in a hospital environment. It is impossible. The system doesn’t allow for it. With the emphasis on reducing liability and facilitating labors which are more efficient for the care providers birth is disturbed even in the best circumstances.
Your hemorrhage chart is a nice graphic.
Because of the oxytocin receptor overload, the teaching hospitals around me are now moving to using prostaglandins as the #2 step in treating hemorrhage.
Thank you Sharon! I have seen this shift too. Interesting how the management protocols adapt to the provider-generated problems. That’s another flowchart.
Please don’t reference “provider-generated problems” and not include yourself (midwives) in the “provider” category. All the midwives that work with our practice are called providers–as are we doctors. If we were only talking about doctors (and not midwives), we would simply say doctors. If you want to blame the doctors, say “doctors.” If you are going to say “provider” be willing to include yourself in that reference, like all NPs, PAs, CRNAs, CNMs, and all other midlevels do.
I appreciate your point Dr. H and that is precisely why I wrote ‘provider’ and not ‘physician.’ Midwives and family practice docs practicing in hospital often employ (whether by choice or obligation) some of the same routine interventions that can contribute to hemorrhage. As do midwives at home, but I would argue far less frequently.
Sharon,
I haven’t yet seen this (prostaglandins) in my area. Unless cytotek is a prostaglandin???? Can you explain how a cervical ripening hormone works in the treatment of hemorrhage? I’m curious! Thanks for your time.
Thank you for your well written article. It is often exhausting to hear so many stories of peril when often times it just doesn’t have to be this way. Personally, I feel far more frightened and at risk of an unpleasant outcome when I am in a hospital. I have had two out of hospital births and two in-hospital births (oddly my last two births occured in an institutional setting). I had to manage my own care with such ferocity while I was in the hospital, that I never really entered that wonderful dreamy stage of labor. Explaining how to catch a baby while mom is on all fours, while you are the mom, just isn’t the best thing for mom and baby. At home I feel like we are working from a place of trust and knowledge that generally mom and baby are healthy. In the hospital, no matter the evidence at hand, I feel that people are searching out difference and complication. Thank you Erin for your article.
Natalie, I can *see* you doing exactly what you describe — instructing the docs what to do with a woman pushing on her hands and knees. How many times have I heard from docs that they can’t “deliver” in that position? Funny, because mothers and midwives seem to do it just fine! Thanks for sharing your experiences!
I know its crazy to think that such intellegent people can’t flip things over in there mind. With that particular birth it was June 24 which happened to be the last day of the med students ob/gyn rotation at the University of Washington (which also means that when my babe needed jaundice treatment a few days later they were fresh med students in peds). I was this doc’s 100 birth, that is why I didn’t get a CNM, and she had NEVER seen an unmedicated birth. Of course she didn’t know what to do, it really isn’t her fault that she isn’t trained in natural birth. When I had my third son, intentionally at a hospital with a perinatologist, he was born completely unassisted because when I pushed everyone freaked out and left the room. I had my husband check for a cord, when he found one I explained how to gently press baby’s head into my thigh and he would just slide out around the loop and I could take care of the rest. When he didn’t start up right away I couldn’t get warm blankets or a bulb syringe without them being thrown across the room at me. My doc, who was running to get to me, just sat in amazement, and when I finally asked for a shot of pit because my bp was low and my pulse was high, and it had been nearly 45 min without a placenta, she was really upset that she hadn’t helped at all. I still got to pay $4000 for the whole thing. I would rather have had my friend and midwife help me out. They don’t throw things at me.
THEY THREW THINGS AT YOU? WTF?
I’m not sure if I’m more revolted & astonished at that, or that this was her 100th birth and SHE’D NEVER SEEN AN UNMEDICATED BIRTH.
“…it really isn’t her fault that she isn’t trained in natural birth.”
I disagree. While it might not have been part of her required training, it is most definitely her fault that she has not taken it upon herself to learn about it.
Agreed! Every professional is responsible for continually learning more about his/her field. In life-affecting fields like medicine, that responsibility is that much greater.
Oh Natalie, I so feel for you!
I was a doula at a birth this sounds similar too. So I can just see this happening.
Wow. Thanks for sharing Natalie. I’m so encouraged reading everything you all have to say here.
For the record, I am a doctor, and I have seen plenty of doctors deliver patients in the “all fours” position…the “mothers and midwives” are not the only people who can do that.
I have attended births in half dozen states and twice as many hospitals over the last decade+ and I’ve yet to see a doc willingly ‘allow’ a woman to birth in hands and knees though I do have a few physician friends who are comfortable with it. They know they are the exception. Perhaps in your area it is more common? I think it is safe to say that by and large most docs are not comfortable with moms routinely in hands and knees whereas as a large portion of out-of-hospital births occur in this position.
This is great. I too always cringe when I hear the “If I had been at home I would’ve died” and I also feel very sorry for the mother. The idea that pregnancy/labor is a condition that needs to be treated perforates all areas of society and it’s such a shame. And who wants to “invalidate” a woman’s birth story, even if she is misinformed? But the truth needs to be put out there! Thank you!
Hillary, while it is a cringe worthy statement most of the time, some of the time it is A VALID STATEMENT. While there are many, many, unnecessary interventions, inductions, c-sections. PLEASE LADIES REMEMBER TO LISTEN TO EACH STORY AND JUDGE IT ON ITS OWN MERITS! We home birthers are sometimes a little to quick to judge this statement!
My nephew was born by C-section, he was born with Sagittal suture craniosynostosis : he had no soft spots, no way to mold his head to the birth canal, No way to be born any other way. With out C-section, they would have had to crush his skull to get him out, or my sister would have labored in vain till she died… But, One or Both of them would have died. Period.
She had a horrible labor, then after the E-C-sec, she was told that her baby had I terrible defect, That he would need to have his head cut open and parts of his skull to be removed (craniectomy) so that he could live.
that he would be in unimaginable pain, and blind from the swelling if he lived though the surgery.
I hate to think of my sister sitting on a park bench, and saying:
“Well if I had stayed at home I would have Died”
I everybody immediately, Judging her. “Tsk,Tsk,” and then not even bother to hear her out.
We that can Homebirth should be light bearers! showing a way.
Everybodies birthstory is worth hearing,, even if it makes us cringe a bit.
Okay, but… a trained midwife would almost certainly have detected that something was wrong and transferred her. While the impatience with the normal birth process in the hospital may have saved her some hassle in this (thankfully rare) case, a planned homebirth wouldn’t have in any way been a death sentence for her or her baby.
For that matter, many women birthing in hospitals are expending so much energy and focus on defending themselves from unnecessary intervention and routines, that they are not nearly as tuned into their own bodies, their baby/ies, and the birth process. It’s amazing the problems you can detect when you’re truly aware of yourself. Our doula told us of the only case of uterine rupture she’d ever seen… the mother was birthing her fourth child (no previous c-sections, either), and suddenly said, “Hm, something’s not right.” It was another half-hour before falling blood pressure led to an emergency c-section, and they found a hole big enough to put a fist through in the wall of her uterus. She knew the moment it happened. (That was in a hospital birth… had she been at home, she probably would have been transferred immediately, based partly on the sudden change to her contractions and partly on her own knowledge that something was going wrong… and would have had an emergency c-section at about the same point in labor.)
The thing is, whether the c-section or other intervention was truly required, or just a product of the hospital’s intervention routine, women without specific risk factors are *still* safer at home. The problems that will suddenly kill you at home before you can get help will probably kill you in the hospital too; if they have to intervene faster than an ambulance can get to your house and rush you in, they probably won’t be able to manage it (especially since they’re so busy telling you that you don’t know what’s going on with your body and ignoring your input).
I disagree that in a hospital setting women are not as tuned in to their babies. I knew before anyone, even a nurse telling me I was fine, that my son’s heart rate was decelerating again. And I was right. Nothing could have removed my focus from him. I am a huge supporter of natural birth but sometimes not so much it’s judgmental followers. With a shortened cervix (<.2mm) I absolutely needed to be very closely monitored and needed a hospital setting, and when my son rolled on his cord unexpectedly, the only thing that saved him was a c-section. Had I been at home and waited to be brought in, absolutely he would be dead. I was only being monitored, no pitocin, no intervention, and then he rolled on his cord. They prepped the OR around the corner just in case but assured me it probably wouldn't happen again. Thankfully they were ready, and when it did happen again he was out in minutes. I will never regret the way he came into this world, and IF I WASN'T IN THE HOSPITAL HE WOULD HAVE DIED. The world is not so black and white, there are always shades of gray!
yes Lindsey, you are right. but as you said, you had a risk factor that ruled out home birth for you. a skilled midwife would not have taken you on as a hb client because of your short cervix.
I totally agree, in my hospital birth, I was completely unaware of what was happening to my body, most of my focus was on fighting with nurses. It was truly awful, and when it came time to push (according to them) I didn’t have any urge to push, they kept telling me I’m not pushing hard enough, and they had to do an episiotomy because I didn’t know what I was doing.
My next birth was an unassisted homebirth, and it’s amazing how different and aware you can be of your own body and birth when you’re just left alone to experience birth naturally.
I disagree with you, Ironica…on our L and D floor, if an emergency arises, we can go from a women in a laboring room to having the baby out in an emergency csection in less than 7 minutes–not to mention that life saving drugs can be administered in mere seconds through your IV. You state that the problems that will suddenly kill you at home before you can get help will probably kill you in the hospital too–can you get yourself to our hospital, into our OR, and have your baby out in less than 7 minutes? Can you push epi or other IV meds in mere seconds in the event that you go into Vtach?
In the story Ironica mentioned the mom knew something was wrong, she was rupturing, but it either was not clinically recognized or was not appreciated for thirty minutes. Anyone who has attended births for any length of time can tell hospital birth stories like this. No one is infallible. Docs aren’t. Midwives aren’t. The system doesn’t always work. Sometimes we loose babies. Sometimes the hospital is the best place for certain babies to be born. Sometimes being at home spares moms and babies significant morbidity. We like to make birth black and white. It’s not.
Such a valid point Stephanie. While I love the idea of homebirthing and plan to investigate it further, I have two such stories in my history. As I was born, I contracted Beta Strep. This was before doctors tested for it prior to birth, so it wasn’t until hours later(after a midwife would have been gone) that anyone knew anything was wrong. Without the prompt care I received(as soon as I was diagnosed I was transferred to an NICU) I would have died. But for God’s grace, I should have died anyway. When my sister was born, she was turned abnormally with her foot twisted in the uterus. I could almost quote Stephanie–there was no way for her to be born normally if Mom and baby were to live. So while I realize that you may often get “I would’ve died!” statements from those that really wouldn’t have, do consider what they have to say. It is possible to have natural, midwife assisted hospital births(all the medications and not-so-good doctors need not be there), so not all hospital experiences need be bad.
Tanya, thank you for your comment. You are absolutely right, hospital birth is not “bad” by definition. I have attended many lovely, low-tech, mother and baby-centered hospital births. Screening and treatment for GBS has become standard, but it is important to recognize that while we have gone to great lengths to “treat” every baby at risk, the mortality rate from GBS disease in the newborn has NOT improved. No less babies are dying from the disease since the implementation of routine screening and prophylaxis.
That is strange, because the American College of Obstetricians and Gynecologists state that there has been a dramatic decrease in the number of neonatal deaths caused by sepsis related to GBS, to the tune of an 80% decrease since the early 1990’s to 2010 when treated with antibiotics during labor. There is new concern about the numbers of women being treated vs. the number of children infected and virus resistance to antibiotics which is concerning, but the treatment/screening does work. It hasn’t eliminated it, but then we were told that small pox was eliminated and we know that wasn’t factual either.
http://journals.lww.com/greenjournal/Citation/2011/04000/Committee_Opinion_No__485__Prevention_of.41.aspx
The mortality rate remains the same for babies who contract GBS, whether their mothers received antibiotics during labor or not. However, receiving antibiotics during labor dramatically reduces the chances that GBS will be transmitted to the newborn to begin with. Fewer babies getting GBS to begin with means fewer babies dying from GBS.
Stephanie, I appreciate your concern, and thank you for your comment. You are right, everyone’s story is sacred and valuable and every woman should have a safe supportive arena in which to share it. It sounds like your nephew was born with a rare condition that, if occurred before the relatively recent development of surgical birth, would have been fatal. We are so fortunate today to have emergency medical intervention available to virtually all women in this country, regardless of whether they begin their labor at home or in the hospital.
Just as another example of “what happens at home” I was doing labor at home. I had been in active labor, post natural water break for 24 hours, at 42 weeks. I started getting very very weak (very suddenly), my bp dropped and I simply was not dialating at all. My midwife calmly and smoothly arranged for a hospital transfer, had my records in hand and called in when we arrived and as it turned out I had a Fibroid tumor blocking most of my cervix at the top and did require a c-section. So I offer instead, “if I were at home, my midwife would have made the decicion that we needed to go to the hospital in plenty of time and without drama.” Home birth does not lead to death when medical intervention is nessesary. Trained midwifes know in plenty of time, probably faster than hospital staff who check on you every hour or so, if there is a serious problem.
“So I offer instead, “if I were at home, my midwife would have made the decicion that we needed to go to the hospital in plenty of time and without drama.” Home birth does not lead to death when medical intervention is nessesary.”
This is brilliant, thank you!
May I offer the consideration that a home birth should not have been attempted because it should have obvious from your prenatal ultrasounds that you had a large fibroid at your cervix…this should not have been a surprise that was noticed when you were in labor…it should have been noticed well before and planned for in advance. Someone was not doing their due diligence, as this would have been obvious and should have been noted much earlier.
I do not support blaming providers for their patients’ choices. Do you really want to go down that slippery slope? Pregnant women are free to decline routine ultrasound. If your patient chose to decline an ultrasound that may have picked up a fibroid I would not accuse you of not doing your “due diligence” when her labor stalled and her baby needed to be born surgically.
Here’s my question. I would love to share this information with people. As a non-mother and a future midwife, I am seen as having a bias with no science to base it on. Is there some place this information is available where it does not come from a midwife? People on my facebook (where I am most likely to share) are very hostile to these sources, saying “well they are just protecting themselves” and “they have an agenda” and all of that. I love how there is an OB (I can’t remember his name at the moment) who is very adamantly anti-cord-clamping that I can link to. Unfortunately, for these other interventions, there don’t seem to be OBs out there promoting not doing them. (Not that I don’t know why.) It’s very frustrating to me.
I appreciate where you are coming from Jennifer. Most of the sources I refer to in my posts are decidedly not midwifery sources. The vast majority of research in maternity care and obstetrics is performed by physicians and researchers in the medical industry, e.g., this study on pitocin exposure in labor. Could you try sharing those studies? Childbirth Connection and Science and Sensibility are excellent resources too.
Sometimes people are too entrenched in their own biases and experiences to consider anything different. Sometimes people feel threatened by the information because they may already be questioning their decisions and do not want to add another layer of judgment on top. But you can help to gently open doors for people, and when they are ready they may pick up little morsels here and there. We walk our own journey, you know?
Jennifer, look up Dr. Alison Barrett she is an OBGYN who is also a LC and a La Leche League Doctor. She has worked in Canada (Ontario) and in New Zealand and is very highly regarded. She is a huge promoter of immediate skin to skin even after Csection and does not support early cord clamping.
I attended a very interesting conference session she presented all about birth interventions and the harm that they do.
Jennifer, look up Dr. Alison Barrett she is an OBGYN who is also a LC and a La Leche League Leader. She has worked in Canada (Ontario) and in New Zealand and is very highly regarded. She is a huge promoter of immediate skin to skin even after Csection and does not support early cord clamping.
I attended a very interesting conference session she presented all about birth interventions and the harm that they do.
Dr Sarah Buckley is wonderful too. An MD who has had 4 homebirths and writes a lot about hormones, the hour after birth and attachement parenting. Her website http://www.sarahbuckley.com has articles and free ebooks. Her published books are great too.
I would like to note that there are plenty of doctors who do not engage in the practices that we are accused of in this post. The only babies that I do not put immediately to a mother’s chest are the ones whose mothers tell me, “Ooo, no, that’s gross. I don’t want it to touch me like that. He needs to be cleaned up.” And with these mothers, I try very hard to change their mind…but I can’t force them to do something they don’t want. Also, all my patients have their baby at the breast within an hour of delivery–again, the only ones that don’t being the moms who refuse to breastfeed.
Failing to hand baby to mom is just one way providers (yes, providers!) monkey with birth and third stage, potentially leading to a bleed. Good to hear you honor the mother and her birth in the way.
Can you comment more on thromboembolism and if or how that would be affected by being in or out of a hospital? I have a friend who suffered from this, though thankfully survived (without her uterus.) She nearly has a heart attack every time I plan another home birth, though she is big enough and kind enough that she doesn’t say anything to try and scare me.
Sure Rochelle. Thromboembolism is tricky — and fortunately it is rare. Careful screening and treatment during pregnancy can reduce the risk, while cesarean surgery increases the risk. Embolism can happen anytime without warning or risk factors; women can die from embolism while in the trenches of a hospital and all its offerings (it’s a leading cause of maternal death IN the hospital). Low-risk women having vaginal births at home have a much smaller risk of embolism. If they presented with a known thrombosis (DVT) they would be referred to a higher level provider and probably begin treatment in pregnancy. I do know two cases of thromboembolism that occurred at home, and fortunately both women received timely medical treatment and were fine. One occurred in the days postpartum, after mom was discharged from the hospital, and the other occurred prenatally.
Thank you for such a thoughtful posting. I have gone back to nursing school to (eventually) become a CNM, as for where we live it is the best option for me as far as legalities etc. People make many assumptions about my philosophies and are sometimes surprised to hear that i am huge supporter of all kinds of midwives and I would love to do home births eventually. But already I can understand the “One the one hand, my inner advocate of truth wants to illuminate the myths and realities of the hospital birth industry. On the other hand, it is her story to tell, her journey, not mine.” and do my best to see where the story is going, but it is hard. I have heard so many stories where i just wanted to bang my head as I hear “Without the hospital and the section my baby would have died!”
I want to bang my head as these people usually do not understand how things got to that point. Yes, even in home births sometimes transfers happen, as do sections. The low rate of sections for most home birthing midwives is NOT due to risk out of clients (as some try tell me) but because of the total understanding of the anatomy, physio, and process that the midwives have – not to mention the patience that they display daily. I wish that more in the general population understood this.
I am having my first home birth with pregnancy number three for many reasons. My last labor I had alot of bleeding problems afterward due to the on call doctor yanking my placenta out and leaving small pieces. Also when I told them that once I
Get to 5 centimeters it’s usually only 30 minutes till pushing they ignored it. Half an hour later while they were saying it would be many more hours I said I thought I needed
To push and the baby was already crowning. The doctor wasn’t they they started rushing around in a panic at least 5 nurses
Were in the room yelling and than the nurse finally told me to push without the
Doctor even there. He wasn’t put on me right away and I developed terrible post partum depression due to the trauma that happend during delivery even though my baby no problems they created panic and started trying
To fix problems that went there
Thank you for the beautiful article!
I find that people who say “I/baby would have died if I’d had a homebirth” often forget an important point – homebirthers don’t have to STAY home (in modern societies anyway). If complications or risk factors present themselves during pregnancy, labor, birth, or postpartum, there is always the option of transferring to a hospital. No one who hemorrhages during a homebirth just shrugs their shoulders and dies – they or the midwife treat the hemorrhage or transfer if necessary. It’s not homebirth or bust!
Thank you Rachel — this is why it is so important for physicians and midwives to be able to work collaboratively. When we have reliable consulting relationships everybody wins! And even when we don’t, women who need a higher level of care are still able to obtain it in this country.
I agree Erin….the ideal being -if you need more care it is easily found- (transfer to hospital). I hate referring to homebirth transfers as ‘Failed Homebirths’ because part of the labor was at home and then you needed what the hospital provided. That is how it should be, a well connected maternity system! I had two HBACs (homebirths after c-sections) that were wonderful. I just happen to live within a mile of the local hospital that would treat me very hostile is I did have to transfer, unhappily. I did take my 2 day old in to check on something I was worried about and was treated horrible, just because he was born at home. This is a disservice to me and my child. Nothing was wrong with him BTW other then slight dehydration…. staff seemed convinced he was defective due to the hospital not supervising his arrival.
Naomi,
I too, abhor the ‘failed homebirth’ label. I think women have enough judgements placed on them, particularly in the language around birth and our bodies. My response is to rejoice for those women who need to transfer. I make a concious effort to make my language as positive as possible. We do not ‘fail’ to birth at home – it is an appropriate transfer of care, demonstrating sound decision making skills by the mother and the midwife. We simply must get beyond placing negative value judgements where none is necessary. For each mamababy to come to birth physically and emotionally safely, sometimes requires more than is available at home. That is not a failure, but a positive and successful use of hospital resources.
Love this article BTW. Often have to bite my lip not to disabuse women of the notion that ‘I would have died’! Womens bodies WORK – they are designed to grow, birth and nourish babies – we have much work to do if we are to change the way girls grow up feeling about their bodies and their abilities.
anyone else have an issue with the statement “you homebirthers/ midwives only bring us problems!!”
I always want to answer “YES!!” emphatically. thats what you are there for!
I have a question. Several times there was reference made to “without significant risk factors”. What risk factors make a home birth a no-go, or *could potentially* make a home birth a no-go? I have a strong desire for a home birth, or at least a birth without intervention…but I have had 2 prior c-sections, elevated BP during pregnancy, and have had several other complications, including surgery at 20 weeks during the last pregnancy, due to kidney stones, and a complete blockage in one kidney. I had a stent placed, which was later removed, and the remainder of the pregnancy was just plain rough. We are covered by Medicaid, and have no insurance of our own, but medicaid covers pregnancy. I know, however, that it does not cover home birth. But I am very, very interested in finding out if this would be an option for me, in spite of past history. I think, with a little urging, I could get my husband to go along with it, as long as we figured out the financial part. Could you shed some light on this for me, or point me in the right direction so that I could have some of these questions answered? I’m a cloth diapering, breastfeeding, somewhat natural-parenting momma’, but I just need some direction when it comes to a decision this huge! 🙂
…I guess I should mention that I have also had two NICU babies due to elevated billirubin levels, blood type incompatibility (they’re A pos, I’m O pos), and possible hereditary spherocytosis. So, if the next kiddos are born with the same issues, we’ll end up in the hospital, anyhow. Still want to give REAL birth a try, though! And honestly, the thought of being with my baby while NOT recovering from a c-section appeals to me…BIG TIME!
And honestly, the thought of being with my baby while NOT recovering from a c-section appeals to me…BIG TIME!
Jessica, thank you so much for your comments. It would be impossible (and irresponsible) of me to tell you whether or not you should consider a homebirth though ;)….What I can tell you is that every woman needs to make the best decision for herself and her baby. Whether or not a midwife would feel comfortable attending you is also, unfortunately, something I cannot answer! Midwifery is regulated (or not regulated) at the state level; most regulated states have very specific criteria for what constitutes “low-risk” and licensed midwives generally adhere to those guidelines (although there may be unlicensed midwives who do not, or certified nurse-midwives attending homebirths who do not have to comply with guidelines governing licensed midwives). Beyond state regulations, midwives have their own protocols and comfort levels so you’d have to dig around and talk to them to see how they feel. Do you have the option of seeing nurse-midwives in your hospital?
That said, having two previous cesareans increases the risk of uterine rupture. Your kidney issue may or may not factor in, that would depend on how your body is working this time around. In terms of the jaundice, well, blood incompatibilities do make babies more jaundice and they may need extra help clearing the bilirubin. In general physicians tend to be conservative with their jaundice management. Some babies do in fact need that care, but by and large babies born in the hospital are ‘overtreated’ for jaundice. Liability issues play a part, as well as the model of care that assumes pathology. We see a lot of jaundice in normal babies at home and that vast majority of them are perfectly normal, healthy babies. You can google “physiologic jaundice” or “breastmilk jaundice and ABO incompatibility.
Meet with a local midwife (or a few of them) early in pregnancy. Most of them have a “getting to know you” appointment that is free. Find out what they think, and then go from there. Even if you decide on a hospital birth, you haven’t lost anything more than an hour or two of your time.
As far as the potential Hereditary Spherocytosis goes…The risk of passing the trait is 50%. It’s estimated that the mild to moderate form may be more prominent than currently detected because HS folks can life relatively normal lives and can go undiagnosed for a very long time.
I was 23 when my son was born (in the hospital via pitocin induction) and he was jaundice within the hour! However, a week of bili-lights, and some test, the hospital and Pediatrician failed to figure out what was causing his jaundice. My son was not diagnosed with HS for 7 more years! The only reason he has been diagnosed is because I pushed for the necessary blood work to be done. Neither of us had been diagnosed with HS. But his birth and “mystery” jaundice put me on the path to figuring things out for myself.
Since my son’s birth, my only hospital birth, I’ve had three daughters at home. The first two did not inherit HS, and the third most likely did (as her osmotic fragility test done at 10 months is indicative of HS). I have HS. My first three children were born while I had a very, very enlarged spleen (which could not be palpated, only an CT scan was able to detect just how large it had become). A year and a half before my third daughter was born, I had an endoscopic near total splenectomy. I also experienced a post-operative splenic vein thrombosis that dislodged and caused a portal vein thrombosis. I was on blood thinners for 6 months!
So, when I became pregnant with my last daughter, I had two midwives who were not quite comfortable with my history, before I found one who was willing to work with me. My daughter’s homebirth went very well, and we both did great! She did develop a bit of jaundice by day three, but it never went past her nipple line (jaundice levels can be assessed by looking to see how far down, head to toe, it goes), and it began to clear rapidly after my milk came in. She has been incredibly healthy and a very fast grower physically and developmentally. The only reason we ran blood work on her was because she was a little anemic at her 10mth check up, and the Ped wanted to put her on iron. I insisted we rule out HS first, and when her labs showed she likely had HS, the Ped dropped his iron recommendation (we had also tested her ferritin aka, iron, which was more than adequate). She doesn’t need iron (which can actually cause damage), but B vitamins and folate rich food.
Get your HS diagnosis confirmed! Then you won’t have to fear it. Most doctors know very little about HS, and if you or anyone in your family has it, you’ll need to be the educator and advocate.
As far as homebirth and HS goes, I feel that my home waterbirths were far gentler, and necessary in helping my HS baby transition into this world easier. Stressful situations can lead to HS crisis, and I do not feel my son’s pitocin birth was the best thing for him. I also believe that HS babies especially benefit from delayed cord clamping, as it gives them the benefits of their stem cells and increased blood volume. So if you are having an HS baby, or any baby in a hospital I can’t stress enough the potential benefits of demanding delayed cord clamping (no cord stripping, as it can damage the cells) and avoiding augmentation of labor.
I am SO GLAD you posted. I have been struggling for 5 1/2 years to have questions answered regarding HS, and have been increasingly frustrated with the few answers that have been provided. I actually had one of the docs in our group of pediatricians flat out tell me that she didn’t have a clue what it is or what I should be looking for because “she’s not a hematologist”! I just about screamed at her ignorance and lack of desire to help me answer these questions. Instead, she preferred that I drive the 2 hours to get to the nearest pediatric hematologist so that HE could answer our questions. We love our hematologist, but he’s hard to understand- he’s foreign, and somehow between trying to understand how he speaks and him trying to “dumb it down” for us, communication is impossible. As far as the 50/50 chance, I was aware of that. The blood type thing is a 50/50 chance, as well…but so far, both girls have both! It’s the combo of the two that has caused such extremely high bili levels. My youngest had a level of 18 at about 12 hours old, and yes, they were both yellow from head to toe! My milk did not come in for 5 days, so with the first one, they PUSHED formula on me, and I was scared to death so I allowed it. With the second, I got smart, got *more* educated, and insisted on NO formula. This time around, I’m going to the hospital armed with 20-30 ounces of donor milk, just in case. I am due in December with my third baby, and I am freaking out already, trying to educate myself on all of this. If you have any more info you can give me, I would be indebted to you even more than I am now! 🙂 Thanks so VERY much!!!
Jessica,
There’s a pretty good group for HS which I’ve been a part of for a few years. Not many homebirthers (I might be the only one), but a very focused group on HS, non-the-less. And you can get ahold of me via my blog http://www.angoraknitter.blogspot.com
http://health.groups.yahoo.com/group/Spherocytosis/
Best of luck!
Susanna
Thank you so much, Susanna! Checking both of them out 🙂
I enjoyed your post. I currently have 4 children and have given birth to the last two at home. I find the setting more comfortable and relaxing, without all the issues of being forced to stay laying down, not able to walk around, eat, drink ect. I have not had issues with hemorrhaging, But my last child was born with a birth defect that was life threatening. After giving birth, he was careflighted from my home and spent 3 months in NICU and has had 8 Surgeries to enable him to breath and function properly. Saying that I am currently Pregnant with my 5th child and will be birthing at home again. I feel that no matter where you go, hospital, home, or child birth center, you may come across something that is unexpected. I put my faith in God, and know that where ever you give birth it should be where YOU are comfortable with. Thanks again for your article.
I guess I am pro hospital. I know that everyone has to make their own decisions. I feel like when you hear someone say “I would have died or my baby would have died. You don’t take them at face value. I wanted to try a home birth and was talked out of it. Thank god I was. I have 4 children and 3 of them were NICU babies who WOULD HAVE DIED! so some people really mean it. My first wasn’t breathing and had to be on a vent for 7 weeks and my twins were vented 3 months. One of them had a pulmonary hemorrhage. Maybe next time someone tells you there story, listen to it not just shake your head and say you understand. Because you really don’t.
Thank you for your comments Traci. I cannot comment on your particular births because I do not know the details. Twins generally are considered to be “high-risk” and most are born in the hospital.
The purpose of this post was not to debate homebirth versus hospital birth, but to illuminate the fact that outcomes in one setting cannot simply be extrapolated to the other, and vice versa.
In some rare cases, yes, babies die regardless of where they are born. And in some rare cases babies born at home may need immediate medical intervention that is not available at home. Typically these are babies with congenital anomalies, which are often detected prenatally.
Homebirth and hospital birth carry a different set of risks. Overall, we do know that babies born to low-risk mothers are as safe or safer at home. In deciding where to give birth, every woman needs to assess the risks to her own satisfaction. It sounds like you made the best decision for yourself and your babies.
I’m reading all the comments and laughing a little because this is my first pregnancy and I have had such a bad experience trying to find a doula. We had to contact 12 of them before we found one who was either available or willing to work with us, and one of them insulted me when I said I would feel safer birthing in a hospital. At the time I recognize I had limited information, however I was open to advice and all I got were insults because of what I felt was the safer option in a slightly higher risk situation. It’s been difficult finding people who are open to the middle road. My ob is a surgeon and that scares me, but so far he has been more open minded to all of my natural birth choices (and I have a whole list on my birth plan) than many of the doulas I’ve talked to who just straight out refused to work with me within a hospital setting. On an end note, we did finally find a wonderful doula who will be my advocate at the hospital.
Women’s journeys through pregnancy and birth are so unique, it really blows my mind. I’m sorry you had such a difficult time finding a compassionate doula that met your needs. I know many are burned out by advocating for women in a system that, in general, does not want them to be advocated for. I have worked with many low-tech, natural birth loving surgeons in obstetrics and I hope yours is one of them. Blessings to you in your birth!
Just to be clear…all OBs are surgeons.
This article is well written and thought out, HOWEVER you barely acknowledge the women with medical conditions who ACTUALLY DO need to be hospitalized or have C-sections. There are MANY women with conditions/diseases/disorders that require C-sections or at least hospitilization for survival of mom, baby or both. There is a reason that SOOOOOO many women died during child birth in the past. Midwives are great and I am very happy that in most states that is still an option for most women out there but midwives simply aren’t equipped to deal with every situation and some (or MOST) of those situations can’t wait for an ambulance (out here the response time is around 20-25 minutes then it’s a half an hour to the nearest bandaid station…err “hospital”). There are MANY women that CAN have VERY healthy and wonderful homebirthing experiences but please acknowledge the women (like me) that don’t have that luxury. Because we aren’t as few and far between as you are leading people to believe (or YOU have been lead to believe). Maybe you should do a post on all of the women who SHOULDN’T be considered for home-birth for clarification on that.
Some medical history so you don’t assume I’m one of those that you dismiss so easily:
baby 1-born at 26 weeks via emergency VERTICAL c-section (1 lb 2 oz) after 1 week on complete bedrest in hospital for SEVERE PIH and HELLP syndrome. Spent 3 months in NICU.
baby 2-seemingly normal pregnancy but baby unexpectedly born with only 6k platelets (are ya’ll trained to treat or even recognize that??? doubtful since you admitted that you don’t “poke and prod” the mother and baby in the hour after birth. ie don’t look closely enough to notice small things that left untreated will turn into big problems.) due to a blood disorder (NAIT-Neonatal AlloImmune Thrombocytopenia) and required blood transfusions and IVIG to save her life. I thank God every day that I had a c-section (obviously VBAC is not an option) b/c without it she would have most likely had a brain hemmorage and either died or been severely brain damaged like so many of the women on my NAIT support group who delivered their baby vaginally).
baby 3-treated throughout pregnancy with IVIG and STILL had low platelets and needed treated (though he showed no physical signs, so he had to have bloodwork done to know this). Also, born at 34 wks due to PIH, etc and obviously also born via C-section.
Sorry I tried to condense it as much as possible lol 😉
Thank you for your comments Renee. The hospital was undoubtedly the safest place for your babies to be born. Beyond the primary conditions causing maternal death, I did not discuss high-risk women in this post because my purpose here was not to debate place of birth for high-risk women, but to illuminate that an outcome in a hospital birth cannot be automatically extrapolated to a homebirth, and vice versa. Obviously cases of life-threatening congenital anomalies are different, and not at all what I was addressing in this piece.
In terms of your particular births, all three were high-risk so none would have happened at home. I am not sure what you are asking?….Your second baby was born with a rare fetomaternal platelet incompatibility that often does not present with any signs or symptoms. In the very rare instance that a low-risk homebirth mother gave birth to a baby with this condition who had overt symptoms — bleeding, seizures, bruising — those are things that would be recognized immediately by a midwife. We may not intervene unnecessarily, but we are always watching. In the absence of any signs or symptoms a baby born in the hospital with this condition would not have had lab work-up performed.
My mother had me and my brother at home (in a bean bag chair), and I have had both of my boys at home. I have heard so many stories of women that were unhappy with their HOSPITAL birth, that I can’t imagine doing anything else. Often when women say “I just couldn’t have done it like that” I think, why not? They have been exposed to the horror stories of their mothers, grandmothers and friends that spent hours laboring with few results. Well, stick a woman on fetal monitors, feet in stirrups for hours, take away gravity, movement and the comfort of home, and add 4 or 5 rotating unfamiliar faces.. why and how would anyone want to bring a baby into that cold, sterile circumstance? I hate, hate, hate that they give children the Vit K eye drops in hospitals immediately after birth, because 1 in 10,000 women might have an STD? Even though if you have been regularly treated, they should know if you do. It steals those first precious minutes of light and life from your childs eyes. With my first son, I got to experience a bright and sunny moment while everyone else slept and we were the only ones up. I greeted what had been a stormy week with a sunny and perfect moment with my first born child. I would not trade that moment for 1,000 doctors assurances!
Tonisa, I love those peaceful, blissful moments after birth. Thank you for sharing that! …..And it is an antibiotic ointment that is routinely applied to the eyes of babies born in the hospital. The Vitamin K is routinely given as an injection to treat Vitamin K Deficiency Bleeding. (That’s another post!)
The statistics of women who have gonorrhea and/or chlamydia in a given year in the US is about 250 in 10,000, with many areas being twice that number. I sourced these numbers from the Centers for Disease Control website (www.cdc.gov). (Gonorrhea and Chlamydia are the STDs that cause the eye infections the ointment is used to treat.) High infection rates occur in both rural and urban populations, and infections are most common in women in their late teens and twenties.
As many as 75% of infection are asymptomatic, and therefore go undetected. I want people to have accurate information about how frequently these infections occur without signs or symptoms so they can make a decision on their PERSONAL risk. You can get tested for these diseases in pregnancy, and make a decision based on the results. (I am NOT advocating for routine treatment of all babies, as the treatment has some drawbacks/risks as well, just for informed choice!)
I realize that this post has nothing to do with the (timely and important) topic of how birth outcomes in a hospital setting can’t fairly be compared to what may have occurred at home. I just have a thing about accurate information when it comes to decisions people make for their newborns!
Hi Erin,
I’m coming at this as an “outsider,” as my two births took place in hospitals, the first with an epidural and the second with no medication. I’m now pregnant with my 3rd, and I unfortunately don’t think that homebirth is an option for me. I have a blood clotting disorder (and a family history of blood clots) that requires me to take Lovenox during my pregnancies. The protocol for someone on blood thinner is to induce about a week before the due date. I guess I’m trying to make the most of my situation. I don’t like the hospital protocol stuff and felt like I was in a hostile enviornment during my natural childbirth experience. I wish I could have the best of both worlds – the atmosphere of a natural homebirth but the immediately available medical attention that I need.
I enjoyed your post, and I have so many questions about all this stuff! First, how long do you wait until cutting the umbilical cord? Also, since the US mortality rate is so much higher than other countries, why don’t we all know several women and babies who have died in childbirth? I know one woman who died after her C-section (she had preeclampsia), but haven’t known anyone else. Who are the women who are dying in our country? Lastly, if you have any tips for someone in my situation, my ears are open. Thanks!
Hi Lisa, thanks for writing. Do you have the ability to see a CNM at your hospital? CNMs can co-manage women with clotting disorders and thrombosis and are much more likely to support at low-tech, instinctive birth.
I am in no rush to cut the cord. There is no need, and in fact is BEST for the baby to delay cutting it until s/he has received her full blood volume. That happens after the placenta has detached. If you cut the cord early the baby is deprived of her full blood volume! At the births I attend placentas are usually born before we get around to cutting the cord. Nicholas Fogelson MD is a public advocate of delayed cord clamping and if your provider is insisting on early cord clamping, Fogelson may be able to provide an alternate opinion. You can find him at http://academicobgyn.com/
The maternal mortality rate in this country, while horribly high, is still low relative to the entire population. The rate is calculated per 100,000 people. Most of us do not know a fraction of that many women. The death rate for non-white women is also considerably — and appallingly — higher. The death rate for babies is higher than mothers, and those of us who work around birth do see it far too often.
If there is anything else I can help with Lisa please feel free to contact me via email!
I never said “I” would have died I said “my son” would have. and yes, I very much believe this. They are absolutely “emotionally charged” statements. That is the reason I did not put them out there until my son was 17 months old. I hate that I truly feel that way because I love home birth. When it comes down to it I have always felt safer with the idea of a home birth instead of a hospital.
It is not that I feel home birth is unsafe. I believe it IS safe however, when i was reading and studying and researching home birth while I was pregnant I feel like the one thing in the home birthing community that is never said is that there are STILL risks. This community is filled with passionate, highly intelligent women who know their stuff and to speak out against them usually results in them tearing you apart (as I have experienced) I knew that when I wrote my post. I think woman who had a bad home birth experience (because yes IT DOES happen) are terrified to share their story. Both hospital and home births have risk and things can go wrong. To say otherwise is ridiculous! You can argue all day about what is the better option BUT you cant argue that BOTH carry some risks. That was my point. I also stressed that I believe home birth is safe but that nothing is completely safe and that it wasn’t to scare but to share, I write honestly. I’m not going to cover up how i feel or what happened.
Thank you for your comments Adriana, and thank you for speaking truthfully! THAT is how birth change will happen in this country. The purpose of this post is not to debate which is a “better” option, or to say that birth does not carry risks. The purpose of this post is to highlight that outcomes in a hospital cannot be automatically extrapolated to a homebirth and vice versa. There are too many variables at play.
You are right, there are risks in any setting, and sadly babies do die. Our maternal and death rate in the US is horrific, and the vast majority of those deaths occur in a hospital setting. Our neonatal death rate is also alarmingly high. I cannot speak to your child’s birth because I do not know the circumstances surrounding your labor and birth.
I firmly believe that our job as providers is to inform women of the set of risks they face both at home and in the hospital. They are a very different set of risks. We know however, that for *low-risk* women, mothers and babies are as safe — if not safer — at home.
Hi all! I love this discussion! I am reading Immaculate Deception at the moment. It was written in the 1970s but still readily applies today and the very subject of these entries. For any one that hasn’t read it, it’s a great deconstruction of the “If I were at home, I would have died” syndrome. It reflects on how we got to the hospital in the first place and how and why birthing women have been “deceived,” stripped of power, control, dignity and self-determination and given and sadly accepted fear, pain and costly (physical, emotional) medical interventions as replacements. (It begins with original sin apparently – oh boy!) It goes on to examine the 1970’s hospital model of care and its outcomes on the mothers, the babies, on the entire experience of birth. What I’ve read so far is compelling and has definitely given more substance to my thoughts about the many ways that we are severed from the experiences of womanhood in our culture. But what’s astonishing?! Reflecting on Erin’s contemporary comparison of at-home vs. hospital birth care philosophies, it seems the general model of treating normal births as abnormal, for reasons that have nothing to do with the mother or the baby’s best interest, still prevails and indeed remains entrenched in our society despite publications like this in existence for a generation.
I am not categorically demonizing hospital births. But I am interested in understanding myself and others within a historical context. I believe that most woman in the U.S. don’t learn much at all about birth growing up, either through experience or otherwise, and are guided by “gut” feelings. But in turn, I believe our “gut” feelings have been tampered with through media’s portrayal of birth as crisis, lack of generational wisdom or ritual, fear of pain, etc. and so the tendency is to see through these lens to varying degrees. In some ways, it seems to me that the debate is less about hospital vs. home birth, and more about about this context and its influence on every woman’s fundamental concepts of being a woman. Where we have our babies would be irrelevant if we all came to expect the same positive experience and model of care. And this is the challenge… It is not entirely easy for some people to accept the inherent risk that “Women can die from birth complications in any setting.” That can be scary and overwhelming, (consciously or subconsciously) especially when our instincts are not universally aligned and feelings of alienation or self-doubt exist. I’m beginning to better understand the additional tasks of the midwife, apart from the direct support of women during childbirth. Midwives have the ability to realign us. They are story-tellers and teachers, equipping women with knowledge about our body’s natural biological, physiological and hormonal functions, and relaying positive birth experiences, wherever they happen. Thank you Erin!
This is the first time I’ve shared my feelings like this, thank you for the chance! I’m a doula-in-training and a midwife to be.
You are so right about the “lens” through which the majority of women in this country see pregnancy and birth. I think there has always been fear around birth, and that fear is normal and actually probably quite healthy. Women can move through fear, and into power and pride in their instincts. Since messages from the birth industry, technology and media have replaced messages around birth that women used to see and feel and experience first hand, and message has shifted from “this will be scary at times and your body *can* do it” to “it will be scary at times and you probably can’t do it. Your gifts as a midwife are many Sonya.
I think that the real point that so many fail to see is that there is not one right way or place for mothers to give birth. It is only with lots and lots of information and an experienced professional (someone properly educated and trained, whether the state recognizes it or not) caregiver that a mother can make these choices. For me, with my first baby, ending up with pre-eclampsia which got severe and having to be induced before I would have gone into labor naturally and ending up with a c-section were things that no one could have predicted, but which I’m sure a midwife would have made the same decisions on… because pre-eclampsia is a true risk.
With my other children, I had VBACs, and could not find a midwife that would do them… they felt that they were something a physician should be present for and none of them worked in the hospitals or they would have still seen me and delivered me there.
However, the choice of the hospital, the choice of the physician, and the choices available to me because of where I lived during each of my pregnancies also contributed. No one wants to develop a life-threatening condition and end up with a c-section, but I have no regrets about the birth… with my second, I wish I had not been in Washington, PA, where I was limited to one hospital, to one OB/GYN practice, and had to fight tooth and nail for the VBAC I had been promised in IL before I moved there.
With my third, we live in Virginia and I had more choices for a doctor… I then also had more choices for hospital, and I chose carefully, choosing one who was very supportive of natural things, who delivered at the hospital that also had a midwifery unit, which meant that even the doctor’s section allowed things that many others don’t. In the end, I went overdue and, because of the c-section from my first labor, I ended up induced, but the doctor and I decided on that together… he told me where he felt he’d let me go, and I expressed my wishes, and he left it up to me.
I pray now that my daughter will be able to only know birthing with midwives and preferably at home, but if she can’t or doesn’t want to, I want only for her to have the information and know the options. Clearly, the problem here is a state repressing the options and the information.
‘I want only for her to have the information and know the options.’
I think this is the main problem with pregnant couples in our society today – they don’t have the information they need. But I don’t really believe that there is an active ‘repressing’ of the options. They are all out there for anybody to find on the Internet!
Unfortunately, there is not much organization in how to find it.
I have tried to remedy this with a site I call virtualpregnancycourse.com. It is designed to help people learn about pregnancy – a subject not covered in most educational venues, make their own choices (with their providers) about how they will handle it, and prepare for a great birthing experience. It is a comprehensive ‘curriculum’ that starts in early pregnancy and goes right into immediate postpartum issues.
I hope it will be useful to some of our current genration of pregnant couples.
Hi There
If a mom begins her story with ““I would have died at home”, listen to her. Nodding and saying “mmm hmm” is not very birthy supportive to say the least.
Mom’s die in the hospital and mom’s die in the home. I attempted a homebirth and was fully dialated in 2-3 hours. My son was posterior. My midwife told me he would come soon and to push. I pushed myself into uterine exhaustion and developed a bandl’s ring (impending uterine rupture). I was the one to notice it out of the 3 midwives that were present. We rushed to the nearest hospital (that wouldn’t have to fly me out) 1 hour and 30 min. away. I ended up having an inverted T incision csection to deliver him (posterior and brow presenting). I suffered from severe ppd for over a year and a half. Educating myself for next baby and allowing myself to grieve is what healed me (not drugs that a dr. would have pushed).
Not every momma’s story is “emotionally charged sentiment”. It’s physical. I am sure some of these mom’s wear the scars on their tummy, hearts and minds. I guess what I am getting at is don’t dismiss a mom’s story because she doesn’t support your view of homebirthing being the best. That is what so many doctors do when they hear the word “homebirth”. They see it as some dirty word, like so many (I use to be included in this) viewed the “hospital”.
The goal should not be to get every woman to be supportive of homebirths, but to be supportive and educated enough to choose natural, intervention free (as long baby is doing ok) births no matter whether they are at home, in a hospital or in a birthing center. The fact is we as women need to educate ourselves about birth. We go into homebirths and hospitals so often unprepared. We need to know the ins and outs of procedures, interventions, herbs, medicines, etc. We need to know what we want for our bodies and babies and trust our instincts.
Homebirth is great if you midwife is proactive and educated enough to know the warning signs of danger.
Just 2 cents from a mom who did almost die after attempting a home birth
Thank you for your comments Jessica. I can see how my description of being on the receiving end of the “I would have died at home” statements could read as dismissive. Please know I do not dismiss your experience, in any way, nor do I dismiss any other woman’s experience of her labor and birth. My own first labor and birth was traumatic, and a part of me may never be healed from that.
You had an extremely rare complication at home that you would have died from had you not received emergency medical care. That is a very real and terrifying experience — one I can only imagine. I am grateful (and humbled) by the amazing heroic efforts of emergency medical care in this country. On the flip side of the coin, thousands of women’s lives have been threatened by unnecessary interventions and cesareans, and missed diagnoses in the hospital. And then there are the women who have tragically died preventable deaths. The CDC has estimated that half of maternal deaths are preventable.
I do stand by my statement that the ” I would have died if…..” sentiment is emotionally charged, regardless of its plausibility. How could it not be? The processes of pregnancy, birth, raising children, and dying are perhaps the core of our emotional being. Can one really talk about their birth, or near death experiences without being emotionally charged?
I was completely honest in this post about my feelings, as the listener, when women tell me how they would have died if they were at home. I feel a double-bind sometimes. I am only human! I do, however, absolutely strive to listen to all women’s stories in deep gratitude, kindness, and love. Always I strive for this. On the clinical side, nine times out of ten (or more), the labor and birth story reveals interventions that caused the complications that the mother endured. That is endlessly frustrating for me (hence the double-bind) not because I am some staunch defender of the superiority of homebirth, but because our medical system has failed women. Women are denied access to informed choice, denied access to midwives, denied the truth about the interventions so often forced upon them in birth. Those are the circumstances I am addressing here in this post when I say that one cannot automatically extrapolate events that occurred in a hospital setting and assume the same outcome would have happened in a homebirth setting. I will add a sentence toward the end to that effect.
Thank you again for your comments. Keeping me on my toes at midnight!
Erin, I am so interested to see what your thoughts would be on whether there’s any reason for me to not have a home birth for my next pregnancy. I wrote about the post-labor complications I experienced here: http://spiritandseed.wordpress.com/2011/03/28/post-labor-complications/
My husband and I are both interested in having a home birth next time, but he especially is concerned. Could everything that happened be treated effectively at home? I think it could.
My concern is that I had some bleeding that caused concern and a big drop in BP, but I didn’t have any pitocin to speed up labor or any medications during labor. I also didn’t experience “interventions [such as] failing to give the baby to the mother immediately, assessing the baby away from the mother, pulling on the umbilical cord, changing the mother’s position to suit the care provider, diverting the mother’s attention away from the baby, clamping and cutting the umbilical cord without any good reason to do so, etc.” My hospital is very natural birth friendly, the baby was immediately placed on me skin to skin, the cord wasn’t pulled on, I was in the position I wanted (delivered on all fours on the bed, then flipped over to hold/nurse baby. The baby was assessed in a bassinette next to me two hours after delivery.
What are your thoughts?
Stephanie, I will look at your link, and let’s try to connect either by email or phone. You can email me at erincpm@gmail.com.
Without knowing the details of your birth, I can tell you that some complications are unlikely to repeat in subsequent pregnancies, especially if they were initiated by provider intervention and that intervention does not occur in the subsequent birth. Subconscious attitudes, either in the mother, family, or attendants can also have a bearing on how a labor birth unfolds — either at home or hospital. And, sometimes shit happens and there is no rational or obvious explanation! Sometimes complications repeat themselves, sometimes they don’t. Some women have a tendency to hemorrhage, regardless of how their labor and birth unfolded. Let’s talk more!
Yes, I had a homebirth with PPH myself- no interventions whatsoever, but I still lost about 1000 ccs. A little shot of pit after birth was enough to get my uterus contracting and stop the bleeding. I would still feel comfortable planning a homebirth again, however, because, as you said, hemmorhage is more likely with routine hospital interventions anyway, and my midwife came prepared at home.
Dear Erin,
I’m an OB/GYN (for 25 years) in the Albany, NY area and have been a staunch supporter of the midwives in my region. Keep up the good work. I admire your clear and intelligent views. The truth cannot stay suppressed forever.
Excellent points. My sister says this all the freaking time, when she was induced, ON HER DUE DATE due to scare tactics and the Dr promptly swooped in and “saved my and R’s life”
For me its “if I had been at home, I would have had a c-section”. I know this sounds CRAZY, but bear with me.
My labor was 28 hours long (or a week and 1/2 if you count the false starts). My babe was posterior despite changing positions and pretty much everything my CNM could do in her power. At 24 hours in labor 48+ without sleep, I asked for an epidural due to exhaustion from the back labor. (Frankly, i was tired of hearing my own screams- hypnobabies did NOTTTTHINNNNGGG). It took me 6 hours to dilate 1cm at one point. My transition? was 3 hours long. Now, had I been at home, and asked to be transferred for pain relief, ALL of the hospitals in our area it would have been an automatic c-section. Either their rates are horrible (45% at one! YIKES) or they’re pretty much against natural birth and basically “punish” you.
My midwife got me the drugs and then let me be. My babe was born 4 hours later. Not naturally, but vaginally. I have gotten a LOT of crap from the NCB community because supposedly its my midwife’s “fault” that baby was posterior. Which is bull. She had me changing positions in labor, before that she gave me the spinning babies website. What a LOT of folks need to know is that sometimes things go wonky, and what the interventions exist is for when they do. They are definitely overused in the average every day birthing woman, but sometimes they are needed. 🙂
I agree, Margaret. I think that your scenario is one where an epidural can be helpful- to give mom the rest she needs to deliver baby vaginally. I’m glad you and your midwife found what was most helpful for you!
My experience was so similar to yours, except mine did end in a cesarean. Even though I struggle with guilt for choosing to have an epidural after 24 hours of natural labor (after being awake for 48 hours), I don’t think I had the energy to endure anymore. When I shut out all the noise of what other people think and just reflect on my experience, I know I did everything I could and made the right decisions. Hearing a story like yours helps to reinforce this for me. Thanks for posting!
I had a similar experience and I REALLY found healing from reading “Birthing From Within” during a subsequent pregnancy. The reasons the VERY naturally birth focused book gave for epidurals totally lined up with mine, and I found a lot of peace and self-forgiveness. Also, I have the benefit of being able to connect with the mothers who birthed in the hospital with an epidural! They no longer feel judged by me as a home birth advocate! All that healing came to a good end when I gave birth at home (epidural-less of course) a month ago. I think sometimes we see other people as judging us, when we are our own worst critics and sometimes need to just relax into our own best decision.
Thank-you for eloquently translating this! I’ve been blessed to have my 3 children all birthed at home, and am currently pregnant and planning my 4th homebirth. My 3 have all been posterior – the positive thing about that, is that i have never known otherwise in terms of long-back-labor experience.
I do get flak from “caring” folks, or other mothers who may feel threatened by my experiences. They preach to me “how they would have died/ their baby would have died if THEY had had a homebirth”, immediately disqualifying themselves and everyone else in similar predicament.
But when people are in a mindset like that, sadly they are not open to seeing it in any other light. Women who choose to birth naturally, who choose to take birth in to their own hands and be an active participant – probably did their share of research. They are seekers of truth and not willing to be spoon fed everything the medical system says as “truth”.
Thank-you, your writing honors our choices and brings value where needs be.
Thank you for this post!!! I’ve been really enjoying what you’re writing here. I had many people tell me the same thing- “You’re lucky you were fine- I would have died at home.” They don’t realize that many of the complications the experienced arose from interventions. Could a baby die at home? Yes. But in a natural, physiologic, low-risk, and carefully watched birth, those complications are rare, and often not much more could be done in a hospital setting. I really appreciate your blog. Thank you for stopping by mine!
Thanks for tackling this issue so eloquently. As a doula I try to do the same–listen with an open heart b/c it is her own journey and story, but it’s important that we talk about it outside of an individual context.
You did a great job tackling a potentially complicated topic.
If I had given birth at home I wouldn’t have had a c/s without adequate anesthesia and I wouldn’t have ended up in ICU in a coma. I’ll be HBACing when I get the chance.
Alayna, your words are making me tear up. I wish you the best in your HBAC journey!
so why back in the days in th 1900s did women die from birth when they were at home?
Many reasons: inadequate hygiene and birthing conditions, lack of access to a medical provider, no antibiotics, failure to breastfeed, poor nutrition and the same complications that kill women even in developed countries today (pre-eclampsia, HELLP Syndrome, PPH, etc). Before the Industrial Revolution, women still died in childbirth, obviously, but child spacing made possible by LAM and tight knit communities with midwives made the likelihood of dying from an uncomplicated childbirth and recovery much lower than what we’ve been led to believe. It was the conditions created by the Industrial Revolution that actually made the maternal mortality rate extremely high in the 18th, 19th and early 20th centuries. The discovery of the germ theory by doctors (something that midwives had already suspected for centuries, and, in fact, the germ theory was first “discovered” after a doctor died and it was noted that he’d had symptoms like those that accompany puerperal fever after cutting his finger during an autopsy that was being performed on a woman who’d died of PF) and its application, as well as antibiotics have made it so that we, thankfully, now perceive dying in childbirth as relatively rare and usually caused by “unpreventable” complications.
Actually, the above is one of the reasons I think this statement is so common. I have had it used about my experience (I had HELLP Syndrome; I know *I* would have been transferred if I’d been attempting a HB because my BP was sky high, but HELLP doesn’t always present with high BP and other than that, I had no symptoms that pointed to it until a CBC was run) and certainly know and have heard of mothers who likely would have died had they not been in/transferred to a hospital. Someone above mentioned that the medical field has trained us well with this perception: childbirth is something pathological and we need hospitals and doctors to treat it. And if something happens because of the treatment, well then thank goodness we were there in the first place. I think that is a large portion of it. I also think, though, that there is a certain type of craving for drama that so many people seem to have. I can’t speak to other countries, but in the US I know we relish the “I was so close to danger” story. I live in Alabama, so this phenomenon is very evident right now. Let’s face it: most of us don’t get up every day thinking that there’s a possibility we could die. And so when faced with the possibility, whether manufactured, imagined or very, very real, it’s dramatic and we tend to believe it. Maybe there’s something in us that unconsciously hearkens back to our cave-dwelling days, a need to feel the adrenaline rush that comes with cheating death. And since childbirth is so well-known to be “very, very dangerous,” it makes sense that many women identify their experience as an “I could have died” one.
Erin, your synopsis of the “I was so close to danger” dynamic is excellent. Thank you!
I think one of the problems is that when we try to have this conversation, it always turns into discussing the back end – what has happened instead of how it could be. Granted, I don’t have a solution, but as I see it, we need to figure out how to educate without making mamas feel like they have to justify their previous experiences. We have to figure out how to keep the conversation on the possibilities of what could happen with a midwife model of care instead of what has happened under the current system.
There is a difference between learning from the past – learning from our experiences – and letting it keep us trapped.
All I ask of homebirth believers is that you don’t judge people who choose to have hospital birth. I personally weighed all my options & felt more comfortable & safe in the hospital environment. I don’t discount anyone’s right to choose what’s best for them. I had an aunt who DID die giving home birth, her child survived; after she died, they had to c-section her baby out of her. So, I defnitely felt more safe, if God forbid I did have a complication that was unforseen & boy did I ever. My cervix never dialated (spelling?). I never went past 1 cm after 24 hours of hard labor w/my first son & never dialated at all w/my second. (Everything else about my labor was normal, progression, positioning of the babies, etc.) I believe it’s not always cut & dry on either side of the issue. I support moms who want home birth & those who don’t feel comfortable with it, I say we all support eachother & bring these beautiful babies into the world with all the love we can. (However they get here)
Thanks for your comment Colette. I hope that this piece did not convey any negative judgment towards women who choose hospital birth. Actually, my first baby was born in the hospital — and it was my choice!
My heart goes out to your family and your aunt’s surviving child. If you are interested in discussing the circumstances surrounding her birth I would be very interested in talking with you more.
The primary purpose of this post was to demonstrate that the sequence of labor events that happen at home or hospital cannot automatically be extrapolated to each other. For example, many women in the hospital never truly get into a strong contraction pattern with dilating cervixes for a number of reasons, and many of those reasons do not apply in a homebirth setting. A few of these reasons would happen in any setting– but not most. So, without knowing more of the details around your birth, we still couldn’t say with certainty that your labors would have progressed (or not) at home.
I agree that more support for birthing women and mothers is an all-around YES.
I really appreciate this post. It’s so clear and makes such an important point. I was just looking into US maternal death today after reading the new Save The Children report (Where Is The Best Place To Be A Mother? And Where Is The Worst? http://su.pr/22vphO )which puts the US last among developed nations for maternal mortality. My sense is that a big part of our problem in the US is extremely poor diet/obesity which can increase the risk of hypertensive disorders. But I know it’s also the interventions that add to risks, especially for mothers (as wrt hemorrhage). I’m wondering, does embolism risk increase with interventions, too?
Yes Ceridwen, the risk of embolism increases significantly postpartum following cesarean section.
I love reading about home births and would love to have my next at home since I had a terrible hospital birth. However, I’m not sure if I’d be a candidate though and maybe you could shed some light since I was led to believe that I would’ve died. I began having issues during my last trimester where I was having dizzy spells and not pain, but a ton of pressure in my head. My bp was 140/90 but I didn’t have protein in my urine so my ob said I shouldn’t worry about pre-eclampsia and that I was feeling this way because I’m little (4’10”) and possibly having a big baby. I was gaining 8-10lbs a week at the end (I literally didn’t have a neck or feet) yet I was eating very healthy with lots of good protein. The ob said I was retaining fluid normally since it was during the summer. I had a doula and I kept a diary of what I was eating and she said it was fine. I went into labor and progressed very fast and was trying for an all natural birth. By the time I got to 8cm, my bp rose so they took a urine sample and saw that I did have pre-eclampsia. I was given magnesium sulfate and though I made it to 10cm, she never came down further than a 2 station. They allowed me to labor down for 6 hours and I pushed for 2 hours but she just wasn’t coming through my pelvis. I believe that because I was bedridden, she didn’t come down. I ended up with a c-section and had to be on the mag sul for most of the next day and wasn’t allowed to be alone with my baby except to feed her because of the medication. I felt horrible! My daughter was very healthy and had a 9 apgar score. I felt that this experience led me to have ptsd and don’t want to go thru another unmedicated labor to end up with a spinal and mag sul again. Would any midwives work with me in the future? Or will I always be labeled a “couldve died” case and will have to birth in a hospital? And what would a midwife do if this situation arose during a home birth?
Trudy thank you for writing. Your story makes me want to scream! What state are you IN? I am really shocked that your OB missed all the red flags prenatally. (I am not shocked that you were fed the “big baby” card.) I wrote a research paper on preeclampsia and hypertensive disorders so I am quite familiar with this issue.
First, the standard of care is to run labs on women whose BP is high, as yours was, especially if they are having unusual symptoms, signs, or “feelings.” Your headache and extreme weight gain are both concrete signs that should have alerted your OB to the possibility that something funky was occurring. If you were my client I would have taken labs and a 24 hour urine (which is the ONLY way to accurately assess how much protein a mom is spilling).
Whether or not to use mag sulfate during labor for high BP is a call that varies region to region and provider to provider. I would say, in general, most docs I’ve worked with will start mag if mom’s BP goes beyond 150/110 in active labor. As for pushing your daughter out, you are right, confinement to a bed is an obstacle to effective, instinctive pushing. There is so much that happens in a hospital that prevents babies from moving down in the way they are meant to, and prevents mothers from pushing normally. It all begins when women are forced to start pushing before their bodies and their babies are ready. This almost always leads to longer pushing times, babies getting stuck, moms get discouraged and exhausted, providers get impatient and exhausted. This is when we see all these forceps, vacuum, and cesarean births that would, by and large, have progressed just fine if the women were left alone to progress normally. This is a great piece on the subject on appropriate “pushing”: http://midwifethinking.com/2011/01/22/the-anterior-cervical-lip-how-to-ruin-a-perfectly-good-birth/
Trudy, I know your birth did not unfold the way you had hoped, but I applaud you for having the courage to ask these difficult questions of your experience! In terms of being a “could’ve died” or “high-risk” case in the future, every woman is different, every baby is different, every labor is different, and every midwife is different. Your heart will lead you to the provider that is right for you. While the risk of hypertensive disorders increases in women who have had them before, they are certainly NOT a guarantee in subsequent pregnancies, and any midwife would be happy to work with you, assessing you along the way for any signs and symptoms that warranted further investigation.
So, the short answer to the question ‘what would a midwife have done,’ if you had signs and symptoms of preeclampsia you probably would have been referred to an OB and would not have birthed at home. If you weren’t diagnosed with PE and did end up laboring at home and had a BP spike, the midwife might have tried some tricks to stabilize or lower your BP if your birth was progressing quickly, which it sounds like it was. At home you would not have been confined to a bed to push, and your midwife would most likely not have pressured you to push before your body was already doing it. Babies come down when their heads mold enough and they are ready. Moms get the urge to push when the baby comes down far enough to trigger that urge. And if you still have any concerns, fears, PTDS stuff, or anything birth-related that you want to process before the next one, I highly recommend Pam England, author of Birthing from Within. She is a friend and my first midwifery mentor way back in the day. Helping mothers through birth grief, loss, and trauma is her specialty. She has a gift!
Let’s not forget that the leading killer of pregnant women in the US is intimate partner homicide.
US is ranked 22nd in the world for perinatal morbidity and mortality just slightly in front of Slovenia. Let’s work together to improve US perinatal outcomes by changing our system of care
Amen to that Annie!
Thank you for this. As a mother, I’ve had a life threatening postpartum complication that required both an unplanned OR procedure and a transfusion in the hours after my baby’s birth. As a midwife, I know I would have been risked out a midwifery care long before the point where I had a life threatening complication (which is why I was in the hospital in the first place). I still confidently attend normal births of low-risk mothers at home and in my birth center.
Actually I really did almost die in a Hospital!! This is why I am planning a VBAC at home. A woman is much more likely to die giving birth in a hospital, than at home.
Beautiful article Erin. If I gave birth in a hospital I would’ve ended up with a C-Section.
Luckily I was at home and gave birth to a beautiful baby boy after 3 days of labor. In a hospital I would’ve been told “…things are progressing…”, “…the baby’s head is too big…”(he was a big 10lb baby and I’m little).
Hospital births are necessary in some instances and a backup plan is important. However birth inherently is not a medical procedure.
What a great post! I sometimes will make somewhat of the opposite comment… “If I had my 1st two in a hospital they would have been c sections and my first might not have made it.” Long story, but she was breech and born not breathing and with my second, the water broke and then nothing really happened for a day or two. That’s way too long for a doctor to wait!
Thank you for this article! You’re absolutely right, homebirth and hospital birth are just so different, and midwives and obstetricians are just so different, that you really can’t say what would happen. A friend of mine had an emergency C-section because her first baby was posterior. Her own research after the fact led her to believe that the C-section wasn’t necessary. Sure enough, her 5th child presented exactly the same way, and she delivered him at home with a midwife. Both mom and baby were fine. The attitudes of her care providers made all the difference in the world.
Yeah you really cant compare home and hospital can you. I often beat myself up for going to hospital for my first and getting swept along to an uneccessary surgery. BUT if I think about it – the chips would have been down against me there anyway. A 9pound VBAC baby came out just fine after laboring in water, and birthing in a deep squat with one knee up. Theres no way the hospital would have “let”me do what I needed to do. So maybe I really couldnt have birthed in hospital.
I was given the usual “your baby would have gotten stuck” line and I believed it myself for a long time. Until I started reading homebirth stories about women birthing 9, 10, 11 and 12 pound babies at home, and women struggling to birth 5 and 6pound babies in hospital that I started to realise its not the size that matters but the ridiculous hospital policys that obstruct birth. I’ve read heaps of birth stories from “would have died”-ers and 9 times out of ten its cord around the neck or baby magically went into distress after epidural or pitocin (“but the Dr said it wasnt related!”).
Whenever you go near this topic you get all these people coming out of the woodwork whose babies “really would have died!!!!!”. Funny then how the stats are so low for homebirth. Yes, SOME really would die. Less than 5%. Not the 30-50% the hospital results would have us believe.
I dont know why people are getting their knickers in a twist about this. I dont think the author is judging – thats exactly what shes trying not to, because yes, without knowing every detail its possible that each new Would Have Die-der you encounter IS correct. Statistically they cant all be though. And as a homebirther you hear this SOOOOO often. Maybe I should go around saying to people “oh noes! if I’d gone to hospital my 2nd baby would have been cut out uneccessarily too” – but I dont because that would be kinda rude.
I support homebirth strongly and I hope to have one (maybe in the future), but after being truly high risk – HELLP Syndrome BP 220/140 liver swollen delivering at 33weeks – I don’t know that I could go back to my dream.
So many doctors label a woman as “high risk” when they really aren’t. This is partly the problem with the “homebirth is safe for low risk women” statement. Apparently, “high risk” now means any remote possibility of something going wrong…and that’s everybody.
It’s sad so many women think they are high risk. Those few who have been truly high risk know the truth about these stupid risk assessments – No matter what you are labeled, you aren’t ready to face the choice of your life or your child’s life…or taking the “both or neither” option. We, nor our families, are ready for those choices and we really don’t recover emotionally from them. Physical recovery is a toss up – a few do, many don’t fully, and the rest die. My doctors were shocked I would not consider abortion after nearly dying. That next baby was my only full term baby. She was born via csection, but we were both healthy. She never left my side and we nursed in recovery. All things considered that was a success.
But I still have my homebirth dreams.
Angela thank you for sharing your story! I think we can all agree that you were absolutely high-risk and thank goodness we have the level of medical care in this country necessary to care for a mom and baby in your situation! I also agree that the use of the term “high-risk” has become quite liberal, and there frequently seem to be an element of pride attached to it.
I agree with this, almost entirely. You can not compare a home birth vs. a hospital birth.
But, when there is a case where mom and/or baby could have truly died, and not due to provider interventions, do you actively listen or are you already nodding along thinking it’s another one of “those” cases?
I ask cause with my first, I almost lost my daughter due to preeclampisa. my bp wasnt “terrible”, but my protein output was “through the roof” (severe preeclampisa starts at about 5gms a day, i had almost double that at 9gms). In 3 days i lost 80% of my amniotic fluid, my daughter had the cord wrapped around her neck twice and she was strangling herself. Her heart rate was bouncing from 160 to 60 bpms, and how frequently she stayed in the low range was becoming more the pattern (we were on the nst for a couple of hours waiting on u/s results). If i wasn’t already at the hospital for a nst & u/s as part of a discharge agreement to go home after 3 weeks in a hospital, i never would have known my daughter was in danger. I had hoped for a water home birth with a MW, but obviously life had other plans, and she was born 6 weeks early and under 4#, but otherwise in perfect health.
Now, don’t get me wrong, my OB/hospital did loads “wrong” with babies #2, my miscarriage and #3 (lack of vbac support, oh yeah), but i take ownership for that. But, that doesn’t change the experience that happened with #1 (which shaped me for #2, and my inability to really assert myself for that vbac). And i know my experience with #1 is not the norm, but to say that when a mom starts a story with “could have died” and you are just nodding away, you totally dismiss them, without knowing what truly happened. And to THAT, i take a deep offense too.
If you can not be sincere, then say so…
Kris, I try my hardest to listen to women’s stories with kindness, love, and sincerity. Maybe you could imagine what it is like to be in my shoes, to be on my end of the conversation. When I say I nod in empathy, I mean it. I nod, because that is all I can do. i nod, and listen, actively and with love, while my brain tries to make sense of all the incoming information. I am only human.
Thank you for such a wonderful editorial on this subject. I am in NC and the midwife you mention has been a mentor and friend to me for a while. I was really sad to watch an episode of “Deliver Me” where a woman was Pitocin induced for over 24 hours then hemorrhaged badly….almost to the point of losing her uterus or possibly even dying. She thanked the doctor a million times afterward for saving her life. She mentioned that had she been “back in the day” she would have been one of those women who “just died in childbirth.” No one ever even mentioned to her that the hours of Pitocin she received made her a likely candidate for the hemorrhage she experienced. They just took her thanks and made sure everyone knew that it was a good thing that she was in the hospital. There are no guarantees in birth….at home or at the hospital. But we know that the more birth is allowed to progress at its own pace and intensity, the less we have to do and the fewer complications are seen.
Erin – thanks for this post, I appreciate your thoughtfulness and the flowchart of interventions leading to hemorrhage. Many people tried to make me feel better after my daughter’s birth by saying, “surely you would have died at the birth center!” I’m the one who says, “mmm hmmm,” to them because I’m not at all convinced.
After 36 hours of labor in the birth center with midwives attending the highly-educated natural birth I so hoped for, after being 9 + cm dilated and pushing for 10 hours, I was transfered to a hospital, where I was given an epidural, antibiotics, pitocin, a vaccuum extractor and finally a c-section to birth my beautiful 10# daughter. A few hours later, I hemorraged 4000 cc’s of blood and had 6 transfusions and 4 frozen platelet transfusions in ICU to get me through. Aside from my relatively older age, and thus my older, tired-from-all-that-pushing uterus, I still don’t feel I would have had that kind of hemorrhage without the above-said interventions.
The “what if’s” are still in my mind and heart, the “you would have died comment” is still emotionally charged for me because ultimately, I still mourn not having a natural non-invansive birth experience for me and my daughter. I may have died in the birth center – we’ll never know – but I still encourage pregnant women to look seriously at non-intervention and support natural birth.
I loved your thoughts,etc… I am a Birth Doula so I love reading about homebirths, natural births, anything. I had my 3 older children completely natural and would have loved to have a homebirth. With my 4th it was natural but when I went into labor at 27 weeks and 20 minutes later gave birth to my lil mirace girl. We were both dying she was way to early and they didnt have time to do anything for us I barely walked in the door before she came. My water broke because of an infection and I went straight to the hospital labor started immediately. They said that my body knew it was in trouble so it was trying to get rid of the problem. My baby. I was bleeding so bad they couldnt get it to stop and I was dying they had to do a immediate hysterectomy. So I can see both sides of the line. It is hard to say if all the stories are true or imbelished. Thank you for your beautiful story! I am going to tell some of my other mommies to read it.
This is not directly related to the topic, I just wanted to make a note about the statistics related to the safety of home birth versus hospital birth, especially since statistics have been noted in this discussion. First of all, we often hear that the number of women who die during home births is lower than the number who die during hospital births. This statistic is not meaningful to me – many more women go to the hospital than have home births, so the death numbers cannot be meaningfully compared.
Second, even if we are comparing percentages of mothers or babies dying, we still need to take into account the fact that women with high risk pregnancies are more likely to go to a hospital (and probably would not be accepted by a midwife – rightly so), and also more likely to die or have their babies die. Unless the risk levels of the pregnancies being compared are equivalent, the statistic loses some of its significance. Also, I wonder – if a woman is transferred to the hospital during problems with a home birth, and subsequently dies, is that counted as a death during home birth or hospital birth?
I’m not saying that the overall conclusions from the data are wrong. Home birth may very well be safer. I just think we need to remember that statistics have to be interpreted carefully if we are to correctly understand their exact meaning.
There are plenty of studies out there that look at the outcomes for homebirths and hospital births that use percentages (so nullifying the whole “but more women birth in hospital so the numbers are skewed” arguement, and that also allow for high risk/low risk dilema. They also make the distinctioned between “planned homebirth”, “unplanned homebirth” where babe arrives before mum can get to the hospital etc, and “planned hospital birth”.
Thankfully, this means that maternal death rates, complications and outcomes CAN be meaningfully compared. Otherwise there is not much point, is there lol? The idea that statistics need to be correctly interpreted, and that there needs to be an accurately compare outcomes is part and parcel of homebirth research (as with any kind of responsible research), because these kinds of concerns are brought up continuously as a reason to dismiss or discount the statistics that show the relative safety of homebirth.
I don’t think this article is saying that there are no risks with homebirth, nor is it saying that there are no women or babies that really are safer birthing in hospital (because niether of those are true, and any birth worker would know that). What it is trying to say is that in the majority of cases, when women say “I would have died at home!!” they are working on the assumption that their labour and birth would have followed the exact same path as it did in hospital – they don’t neccessarily understand that how their birth was managed in hospital is very different to the care they would have received at home, and that there is a good chance that any intervention or complication they experienced in the hospital would have been avoided or handled differently at home.
This article really isn’t a judement of those women who say “I would have died at home”, because that would be unfair, and unsupportive of those women – its a commentary on how different the models of care are, and how concerning it is that care that is based on policy and business (much higher up the chain than midwives and doctors) often creastes the very problems that they go on to “save” women and babies from.
“Unless the risk levels of the pregnancies being compared are equivalent, the statistic loses some of its significance.”
Correct, and that is why research on the safety of out-of-hospital births compares low-risk homebirth to low-risk hospital birth. Medical research is conducted by folks adept at statistics and epidemiology, that is their job. (And thankfully not mine 😉
To read the largest prospective study about the safety of planned home birth and also the press release the Citizens for Midwifery wrote about it, follow this link:
http://cfmidwifery.org/resources/item.aspx?id=84
The study was published by the British Medical Journal in 2000, and compares planned home birth in a low risk population to planned hospital birth in a low risk population, and takes in to account the difference in the number of people choosing birth at home vs. birth in a hospital.
And yet ACOG says there’s a 3x increased chance of death with a planned homebirth — and homebirthers are ONLY supposedly “low risk” patients. Do you think they pulled that stat out of the air?
No, they didn’t, just as the head of ANZCOG here in Australia says there is a 3x increased chance of death in planned homebirths, and cites a Western Australian study to support it. What he fails to mention is that all but one of those 6 deaths were not related to the place of birth/labour – the babies were unfortunately known to be incompatible with life, and would not have survived no matter where they were born. The other poor babe was so ill there was very very little chance that being born in hospital would have made any difference. That important, and tragic, information was left out of his statement, for reasons best known only to him. This is why doing the research is important. Knowing how the studies have been carried out, and what they *actually* say is integral when talking about the validity of someone’s statements.
I agree that homebirth is safe or safer than a hospital but only when hospital transfer is available. If there is no option for medical care it can be risky. Ever see the documentary about fistulas in Africa? Throughout history moms and babies have died during birth. I think homebirth is great and it’s the way we were meant to give birth but one should know that birth isn’t without risk and that women with no access to healthcare arent just spitting em out like pits but do sometimes run into some very devastating circumstances.
I am very aware of the women suffering from fistula in developing nations. VERY. The reason fistulas are uncommon here in the US is that women are not forced to suffer through an obstructed labor without medical care. In areas where women lack basic medical care and care during labor, some cases of obstructed labor would have been avoidable with the availability of simple midwifery care during labor, while other mothers may need surgical intervention (cesarean). When we talk about the safety of homebirth, we are talking about women who have skilled midwives and who have access to hospital care when necessary.
As stated many times above, great article. I enjoyed 4 wonderful homebirths before my 5th, which ended up being in the hospital. Our midwife advised us to go due to developing symptoms. Long story short, our son was born with unforseen health issues, and everything turned out well in the end. I know that he would not have survived without medical intervention, and realize that his life was in just as precarious a situation at a hospital. With that said though, this is truly the exception and not the rule. As observing/participating in 50+ births, and with many friends/family members having babies, I have heard varying emotions on both ends of the spectrum. I hate hearing the “rescue” mentality (some dr. overreacting or just plain causing the complication) and the mother’s eternal gratefulness for her doc (like the brick thrown through the window with an add for a window and glass company advertisement!). Just as equally, I love hearing the stories of overcoming, family intimacy, and empowerment of moms who did it the natural-loving way.
Something that’s often overlooked in these “I would have died” stories is that you can go to the hospital if something comes up. These stories often assume that homebirth means you stay at home no matter what happens and/or that there’s absolutely nothing a midwife can do about hemorrhage, a slow-starting baby, etc. It’s also often assumed that a midwife doesn’t monitor the baby or is only there at the very end to “deliver” the baby, since that’s what the doctor does. These are, of course, not true, but the women telling these stories think homebirth means having no idea what’s going on in the birth and eventually a baby shows up and hopefully breathes and if s/he doesn’t or the mom bleeds too much, well then they just die and there’s nothing to be done.
My second birth ended in a transfer. She was a single-footling breech and if we had stayed home, yes, eventually both of us would have died because it wasn’t possible for her to come out vaginally. But guess what, we didn’t. Because we got up and went to the hospital! Despite the C-section under general that I ended up with, I am still glad we started at home and I am still very much pro-homebirth. With a transfer plan in place and a good midwife, babies are lost just as often and mothers are lost less often than in the hospital. And thankfully, these losses are rare in both locations!
I live about ten minutes away from my hospital. The emergency services ought to get there pretty quick right? But when my little boy had an allergic reaction to peanuts the ambulance took 35 minutes to get to my house. I waited ten minutes and then I put him in my car and drove. I called my husband when I got to the ER, the ambulance still wasn’t there. He estimates they arrived about 10 minutes after that. A woman bleeding to death or an infant not breathing does not have that kind of time, so saying blithely that you can just transfer as if it is easy as beaming up is really inaccurate and can potentially do grievous harm to women who might be reading your comment. Every moment counts. I do support homebirth and a woman’s right to choose but minimizing the risks is really inappropriate.
I don’t necessarily agree that a home birth is safer than a hospital birth, but I definitely agree that a low-intervention birth is safer than one with the traditional interventions/medications. My pregnancy was considered probably medium-risk because of the medications I had to be on to control my ulcerative colitis, so I was closely monitored by my OB. I wound up switching to a CNM at 33 weeks because my OB was intervention-happy (wanted to induce on my due date, etc.), but we wanted a Bradley birth. I know I would have wound up with a C-section if I’d stayed with my original doc, but my 41 hours of completely drug-free labor (baby was a surprise occipital posterior) and birth were GREAT in the hospital with our midwife! I’m glad I had my first in a hospital since I didn’t know how I would labor, but I wouldn’t mind trying for a home birth next time, if I can find a midwife who will work with me. (I think mine only does hospital births.)
By the way, THANK YOU for such an excellent article!
I, for one, hemmorrhaged right here in my own home on my own living room floor after a beautiful homebirth experience. The immediate and talented (yet gentle and quiet) response of the CNM’s attending me makes me a mother who is proud to tell her homebirth story to any and all who want to hear. I was well cared for in front of the fire burning in my living room with my sister and mother watching over me and my newborn son. Although my son was placed in my mother’s arms as soon as the bleeding became severe I was able to see, hear, and even reach out and touch him during the next 30min. I was told I lost approx. 800cc of blood. There was no drama, no yelling, no bright lights, and no coersion to accept anything I did not want. I was gently informed that an IV for fluid replacement as well as methergine and oxytocin were imperative. In a truly ethereal moment one midwife coached me to think of my body and believe that I could form a connection to the bleeding and envision it stopping. Her few moments of magic distracted me from the needle pricks in my thigh and forearm from the second midwife. They worked quickly with amazing precision and very little verbal communication between them. While the bimanual uterine massage was uncomfortable, I knew the treatment was necessary. I closed my eyes and breathed deeply while blowing out through the pain. When I opened my eyes, I was surprised to see the reflection of my own tears in those of my midwife. She told me weeks later that she hated having to “hurt” me. I am able to type this today because of a team of midwives that became angels in my eyes the morning my son was born. My birth experience was everything I had ever hoped for and I wouldn’t dream of having a moment of it occur any differently. I am blessed to have found such wonderful women who were able to treat me with kindness, respect, professionalism, and the wealth of knowledge they possess. I WAS AT HOME AND I DID NOT DIE!!
Theresa, that was a lovely post. {hugs from a midwife}
Thanks for being sensitive to mothers who have had bad experiences. I chose a hospital birth, but did my best to go natural. After a really slow rough labor that lasted 31 hours, I ended up having a cesarean because my daughter’s head was tilted to the side and would worsen every time I pushed. I support home birthing and plan on trying for a natural v-bac now with my second pregnancy, but I struggle so much with guilt and it’s often not helped by articles like these. Many home birth advocates unintentionally pour condemnation on women who have chosen hospital births. I feel like you’ve written a piece with honest truth about the effects of hospital interventions, but also not made me feel like a total failure for using some of those interventions. Thanks for being a gentle voice in a world of shouting.
Hi Jessie!
I’m a midwife that just happens to be browsing this blog tonight. : ) Malpresentation is a real problem in birth. Sounds like your baby was asynclitic. My baby boy did the same thing! Good for you for working so hard to have a natural birth. Sometimes it’s just not in the cards for things to go perfectly. Although we can use all kinds of position changes, etc., they do not always work. I did end up needing a cesarean (which was hard, as a midwife).
I think what this article is *mainly* about is that normal birth *hiccups* can be exaggerated into life threatening complications (depends on your perception) and the fact that some birth complications can simply be avoided by staying out of the hospital.
A few examples that I hear ALL THE TIME are: “cord was around my baby’s neck” (99% of the time it’s a NON-issue, but a good excuse for docs to use to intervene), “I bled a lot after the birth” (were you induced??? did you think a midwife couldn’t handle a hemorrhage???), “I had to push for 6 hours and his head got stuck” (were you induced, on your back, or with an epidural like most of the population???), “my baby had fetal distress” (were you being induced???), “I had a BIG baby and had to have a c-section or we both would have died” (really??? I caught two 11 1/2 pounders last year with no problems), “my baby didn’t breathe and the had to help him or he was born blue” (midwives see this frequently and know how to stimulate babies to breathe), etc., etc.”
This article does NOT apply to mothers that would be considered high risk in a normal home birth environment. There will always be complications that require proper medical assistance. Thank goodness our docs are trained in c-sections, etc. and have the knowledge to treat our women that do have serious complications.
Most complications can be recognized by skilled midwives and dealt with accordingly.
Can all women deliver safely at home? No. Your midwife will be able to tell you who is considered high risk.
Thank you for your educated reply to this article. I was one of the high risk ones who could not have given birth at home. After 10 years of losing pregnancies, I finally found a doctor who cared enough to figure out why. The pregnancy was going pretty well until at 36 weeks my water broke and after most of the day my cervix would not open. After having her I had a rough time with post partum depression as well and since my biological mother committed suicide 8 weeks after I was born, I was so thankful for a wonderful group of open minded, non-judgemental women doctors. I can think of nothing worse than having someone trying to make you feel like less of a woman just because your body didn’t work properly.
I would generally agree that most women in home birth or out-of-hospital birthing center births are safe, and when complications do arise, they can generally be transferred to a hospital with enough time. However, I now know of three babies born either at home or in an out-of-hospital birthing center for whom the same cannot be said: two of the babies died, one is severely disabled. With babies, even if it takes only a few minutes to get to a hospital, if things have gone wrong, those few minutes are a few too many. Don’t get me wrong, I support midwifery and the idea of home or birthing center birth, and I think women generally come out better for it, but it must be acknowledged that babies are the ones who are at risk in these situations, much more than the mothers, I think. And, even if they are unusual, you only need to have one friend grieving the loss of her baby, for you to really think hard about whether or not your own comfort as a laboring mother is worth it. For what it’s worth, I had a pleasant enough experience (for a really hard labor) giving birth without pain meds with a midwife in a local hospital. I originally chose it because a cousin of mine was born with some unforeseen birth defects that required immediate care, and it felt more comfortable to me to be in an environment with immediate back-up care. Also, the idea of screaming in pain in my thin-walled apartment with nearby neighbors didn’t thrill me. Knowing of these three women and the outcome of their births now (all after my own labor), there’s no way I could consider a home or out-of-hospital birthing center birth. Overall, I think it’s a shame that the experience many women have had with doctors or hospitals has pushed them to a point where they feel forced to have children out of reach of very excellent emergency care if they or their baby need it.
“And, even if they are unusual, you only need to have one friend grieving the loss of her baby, for you to really think hard about whether or not your own comfort as a laboring mother is worth it.” Frightening things do happen and it is definitely scary when they do. I completely understand your fear after having friends that had such heart breaking experiences. I cannot imagine what that feels like! My heart breaks for all of the mamas that have had to go through that. However (and I’m not totally negating what you said), it’s not all about the mom’s comfort.
Again, I am so sorry that these women had to go through that. Hashing the experience out won’t help those families feel better. Since we are having an open discussion, though, were these babies that died born in the hospital or at home? Do you know what happened? It would help bring light to your story a bit.
Two were born at an out-of-hospital birthing center one at home. The one whose mother labored at home for a home birth was taken to a hospital when it became clear the baby was in a position where the midwife/mom could no longer do anything to make him descend and his heart rate plummeted (the mom had had a previously uncomplicated birth). He was born during emergency c-section and his survival was called a miracle, although now has severe cerebral palsy. I believe he was oxygen deprived for around 8 minutes. Another was born at an out-of-hospital birthing center. Two weeks late, 7 hours of pushing (I know some midwives are OK with this, but after my two harrowing hours of pushing out a posterior baby, I find this somewhat of a red flag), and the baby was born with so much meconium in the lungs that she did not survive the three-minute trip to the nearby hospital. The third I’m a little less clear on details (not everyone wants to talk about these things), but a similar situation as the second, a difficult labor, baby born in distress, out-of-hospital birthing center could not revive her. Died en route to the hospital. It’s obviously one conclusion that these midwives missed signs that these ladies needed an earlier hospital transfer (a theory I’m partial to on the second, at least). And I do know several wonderful women who have had multiple home births with no complications, so I realize the deaths are the exception, just a hard one to see happen.
“I think it’s a shame that the experience many women have had with doctors or hospitals has pushed them to a point where they feel forced to have children out of reach of very excellent emergency care if they or their baby need it.”
I agree, that would be a shame. However, I think very few women *are* out of reach of emergency care if needed, and even fewer would decline emergency medical care if needed.
I cannot rightly comment on the cases you mention without knowing more details. We do know that our infant mortality rate in this country is regrettable, and that every day babies are born compromised and injured on account of procedures and medications that have become standard in obstetrics, and that some of these babies do die. The vast majority of babies born with CP and Meconium Aspiration Syndrome were planned hospital births. It is always heartbreaking when a baby dies, especially if it appears that the death was preventable. Birth is not without risk. There are risks in both homebirth and hospital birth, but they are a different set of risks, and women need to be able to make an educated decision about which set of risks they are comfortable with.
Very well-written article. I appreciate your objective comparisons. I’d like to ask a serious question as it relates to the birth of my 3rd child. Having had two previous babies born at 36 and 37 weeks, after 4-6 weeks of preterm labor and all the intervention that goes along with that, the third time I made it to 38 weeks. Had my very first epidural (never had enough time with the first two) and I’m glad for it. Turned out baby began having big decelerations in heartrate with every contraction; her heart beat began to slow down too much and Dr. informed me he wasn’t going to wait, and used forceps to get her out. The cord was wrapped twice and knotted around her neck. Yikes! How would such an event have played out in a homebirth? I wasn’t in any danger but my baby was. I’m genuinely asking: what might have happened?
It’s wonderful that you carried the baby to term!
Several interventions could have helped the situation if at home. Position change, oxygen, emergency (necessary) episiotomy to aid in delivery, or disengaging the fetal head by pushing the head out of the pelvis (allowing time for transport), medications to stop contractions (if the midwife has orders) allowing time for transport, squatting to quickly push the baby out would have been a good choice and probably just as quick as forceps for someone having their third baby (but it’s something that can’t be done with an epidural).
Jen, it’s always tricky to ‘armchair quarterback’ a birth, but Kristen addressed some of the things that might have happened had you been at home. Quite a lot of babies are born with cords around their necks — multiple times — and even with knots, and most of the time they do fine, though sometimes the cord does cause dips in the fetal heart rate in labor that put gray hairs on our heads. Sometimes the drop in heart rate is transient, the baby recovers well, and sometimes it warrants transfer to the hospital in case a higher level of care (or surgery) is needed. In your case, you also had an epidural which we know puts the baby at risk of heart-rate decelerations as well. So, was it the cord, or epidural, or both? We can’t know! If the heart rate fell into what we call a “non-reassuring pattern” and did not improve with the tricks Kristen mentioned, and the birth was not imminent, the hospital would have been the safest place for your baby to be born.
Hi erinmidwife : )
I hope you don’t mind that I’ve been chiming in tonight. This article keeps getting posted on my FB wall and I had a few minutes to join the discussion.
Please chime in! That is the purpose of a comments section! I’d like to reply to everyone who posts but I don’t have that kind of free time. I am glad you’re able to address some of the issues people are raising.
Thank you for your wonderful article. I am a doula and everyone loves to tell me about their births and how they or their baby nearly died only to be saved by the doctor who showed up in his super hero scrubs with his DR. badge over his left pocket and of course he was encircled with a bright warm glowing halo of light. (or was that the exam light?) Anyway, when I was new to all this it was hard to listen to “If I wasn’t at the hospital my baby would have died!” stories. Especially when the next words are something like, “His cord was around his neck and the doctor saved him! So he would have died if we had stayed home.”
I also like it when the doctors say something like “Good thing you were at the hospital! Having pit after your placenta released saved your life!” What the doc always seems to not mention is that if he hadn’t been applying a little “manual traction to help the placenta out” she probably wouldn’t have needed the pit anyway. (Yes I saw a doc do this!) or my own experience of “breech babies never turn. You’re going to develop complications anyway, so we might as well do your c-section today at 36 weeks! Besides I would hate for those complications to develop this weekend — I have a golf tournament!” I thought at this point he was going to kill both of us so I left and had my first HB four weeks later on my due date.
What I have learned to do with these stories is keep my mouth closed and just validate a mom’s feelings. She really is just looking to feel good about the choices she has made. This is sort of a defense. A “look my choice was better than yours because…” because she needs to feel better about what might not have been the best experience for her in many ways. I figure there are other times to educate someone. Yes there are those days I SO want to say something like, “Oh it’s so wonderful that you had a man who can call himself a hero to his adoring fans to feed his ego. You know those home birth folk just have uneducated witches with long dirty fingernails who call themselves midwives at their births. They certainly wouldn’t know anything about unwrapping a cord or clamping and cutting it.” But this just wouldn’t be helpful and might actually be harmful.
I also can praise hospital birth when it is needed. A hospital really DID save my baby and I. Without an emergency c-section I would be dead as would my baby. We had dry Eclampsia. Basically, I had no warning symptoms. I was even retaining less water than I do when not pregnant after someone brought over KFC. BP was good the day before and 3 days prior no protein in the urine. Then I woke up not feeling well. In less than an hour I had the worst headache of my life and saw flashing lights like when you see stars. I had just enough time to lay down and tell my husband I don’t feel well I have a headache. I never got out the part where I asked him to call an ambulance before I lost consciousness. It REALLY is NOT fun waking up something like 18 hours later in ICU but it beats the alternative of NOT waking up. I also had to endure a LOT of criticism that “this wouldn’t have happened if you were at the hospital.” I finally looked at this doc w/ his gaggle of med students and said if I was at your practice and presented like I did would you have done anything different? When I peed into the cup and there wasn’t any protein, my BP was normal and my rings and shoes fit would you have done a CBC? He responded, “Honestly, no there isn’t anything different that I would have done. I have to tell you we see maybe one or two cases like this every 2 or 3 years among the three hospitals. They scare us all to DEATH because there is nothing that we can do and usually the mom and baby don’t turn out like you two. All I can say is God really wants you and that baby for something. He really must have a plan for that baby.” I think this hits the nail on the head. Doctors REALLY do NOT like things to be a surprise. They like to be in control. They like to be able to predict a problem before it happens. Yes there are always accidents but most of the time you can look at a situation and fit it into a box and make a pretty good guess at what is going to happen next. I think this is why many times they want so many interventions.
I am in the “baby would have died” category. I was pressurised into being induced and not warned of the consequences. Things went horribly wrong and after being treated badly by hospital midwives, my concerns dismissed, my birth plan never even glanced at it ended in emergency c-section. I am told the cord was twice around her neck and once around her body and she would not come out, that she was facing my back too and that she must have been in that tangle before I was induced – I will never know! I would love a home birth for this baby I am carrying but am “high risk” and nervous, my husband is even more unsure of it as hospitals are seen as the ‘normal’ way to birth. I was lucky last time being able to bond and breast feed my daughter, I value that so much and don’t want to risk loosing that next time – it is a confusing and fearful world for a mum who doesn’t know what to do for the best
Louse, there are vast resources online for VBAC mamas. Are you familiar with ICAN? There is a world of support and resources out there for you!
No one needs to feel sorry for me for saying “If I had been at home I would have died.” I would have and so would my child. My water broke 4 weeks early and I was having contractions about 30 minutes apart. After 17 hours my cervix would not open at all and my daughter’s heart rate had bottomed out. (any ideas how to pop out a kid with no hole to pop ’em out?) So very thankful for my doctor, the c-section and most of all my beautiful, healthy, happy baby.
Not all hospitals and doctors are horrible and only out to make a buck. I had one of the best groups of women doctors in the south. And after 10 years of misscarriage and heartache, I am so thankful to be able to enjoy the title of mom.
Try not to be so closed minded.
I don’t feel that it’s a matter of being close minded. I don’t think there is a midwife out there that would say you should have had your baby at home under those circumstances. The midwives I know have a back-up OB they work with in case they do need to transfer.
I would say you got lucky with the group of doctors you had and were in very capable hands. I don’t think the statement that she was making is all doctors/hospitals are horrible…but for the US to be so developed and yet have 40 countries above us with fewer maternal deaths should say something. Of the births I’ve attended they’ve all been in a hospital setting…and the women that wanted a natural birth had to fight tooth and nail to not be messed with, heck to just stay out of the bed. If things are progressing normally and safe why should it be so hard to get what they want and could safely have?
Hospitals are for people that are sick or need help. You and your child did and that was the right place for you to be….I didn’t, but I was young and hadn’t been given an option….my first 2 births I felt powerless and unhappy…the 1st was horrid. Though I did get two healthy boys, I was not happy w/the labors. If I’d had known midwives were still around I’d have had them at home too. The women I’ve worked with had no clue what was going to happen with them. When the heard they would be recieving pitocin, epidural and bed went right with it….neither are true. If OB dr.s want to be seen differently then they need to start completely and accurately informing women about EVERYTHING!
Just because “we” dont’ feel all births should take place in a hospital, those should be saved for those that need the help (like yourself), doesn’t make us closed minded…maybe more open minded actually….as we are willing to look at an alternative to the hospital, the way women for 1,000s of years have done. (And now with the option of medical help if needed.)
And, just forsaying sake. If you had had a midwife, with you being that early, most would have taken you to the hospital. Those that would have had you labor at home would have been keeping an eye on her heart rate and transfered you at the first sign of trouble. Especially if you’d labored for 17hrs with no cervical change and heart rate dipps.
(I’m glad you ended up with a beautiful healthy daughter….I know miscarriage is heartbreaking.)
Mama, please know that no one here is judging you, least of all me. If your water broke prior to labor when you were 36 weeks, your midwife would have transferred you to OB care in the hospital. Had you not had midwifery care or obstetric care at that time, then YES, you may well have a very different labor and birth…. And had you planned a homebirth, and your labor did not progress normally, you would also have had the option of transferring to a hospital.
I love the article and the discussion!
I’m one of those who *would* have had a c-section with each of my births if I hadn’t had a CNM. I was in a hospital setting, but completely support home-birth options. I know how difficult it was, even with a midwife, to advocate in the hospital for the births I wanted. My husband is a nurse practitioner and my Mom an RN and it was still difficult at times. Only with my third did I feel completely supported, with no pressure or questions asked.
Even the OBs I know admit they would have intervened, “needed” to due to “liability.” If they had they would have messed with three ultimately perfect deliveries.
This was wonderful to read on the level that I am a doula and have had both hospital births (my 1st & 2nd sons) and homebirths (3rd & 4th sons). The difference is mind boggling. Even just the little things that I remember: my midwife would wait to check me (the 2xs she even did) until the contraction was done…OBs wouldn’t, I guess they didn’t have the time to wait. I remember hearing the nurse tell my family after my first son’s birth to make sure I don’t fall asleep with him where a midwife puts you to bed with your child. FYI: I slept with all four of my sons from the time they were born and never once rolled over on or killed any of them. (I’m not saying it doesn’t happen and please accept my condolences for those of you that it has happened to.)
I became a birth doula as my first stepping stone to becoming a midwife. I know the difference it makes having someone there that believes in you and your (body’s) ability to birth your baby. Women need to have faith in themselves. I am new to the doula world and have attended only 4 births, but I’ve already had to deal with the crap the hospital system (some OBs included) pulls. And I’ve watched four strong women travel the road to motherhood, all with their different obstacles….and they should all be so proud of themselves.
W/ my 1st I was induced because I was 4 days late and my BP was a little high. I was given pitocin for hours & not allowed to get out of bed or move around….so that led to a shot of narcotic that did nothing but make me tired and unable to sleep…which eventually led to an epidural. I pushed for 3 hrs, but had him vaginally. (20hrs long.) My 2nd; I went into labor on my own & went to the hospital after 9 hrs…the nurse told me to get in the bed until the dr. came in…45 minutes later my labor had stalled…so I was given pitocin again (not sent home or told to get up and move)…..later came the epidural. I pushed three times; they had let me labor down this time. (18hrs long.) I hadn’t know my options even though I’d taken a childbirth class. And I didn’t feel I had any SAY in my care or what I did…the OB had our best interest at heart, RIGHT? My 3rd; at home…need I say more. ( : I didn’t know what real labor was like. When my BODY started to push I thought I was going to throw up not have a baby. I didn’t push once, my body did. (6hrs long.) My 4th; at home again…it took a little longer as he was very close to #3 (only 15mos apart) & my muscles weren’t quite back from the last. (10-14hrs long.)
STAY STRONG AND HOLD OUT FOR WHAT YOU REALLY WANT.
HOMEBIRTHS ARE SAFE…HOSPITALS SHOULD BE SAVED FOR THE SMALL
PERCENTAGE THAT NEEDS MEDICAL ASSISTANCE.
I would trust a midwife to deliver my child before I would an OB,
maybe that’s why….I’m not sick, just having a baby.
This was an awesome post that really shed light on how I often feel when I hear my friends rejoicing over upcoming inductions or making those I could have died comments… I so very much want to scream “NO” don’t do it when it comes to induction.. Because one intervention seems to lead to another and another and although I can relate to the impatient feelings that seem so overwhelming at the end of pregnancy I only wish I could steer them away. And yet I feel like this huge discouraging force trying to steal the joy they have in meeting their lil ones or the joy they have in telling their story. I myself endured two inductions leading to cesareans before having a successful vaginal home birth. So I know from experience how things progress in the hospital. We are in instant gratification society and unfortunately many of these so called birthing complications are induced-complications and would not occur in a home setting.. Anyway no more reason to preach to the choir but thanks again for putting these thoughts into words!
I think that the discussion is good, but many women are missing the point. Please read the comment where the woman says something like “If I were at home, I would have been transported to a hospital when the midwife realized that it was no longer safe to remain at home.” If you are at home, there is no reason to stay at home if things aren’t going well.
“You can’t simply cut and paste all the circumstances surrounding a given hospital birth, superimpose them on a homebirth setting, and predict the same outcome — or vice versa. ”
That’s exactly what you do in this article. You take the circumstances surrounding an augmented hospital birth, which ends in PPH, and you say “well that won’t happen in a MW attended homebirth”.
Great post, adding this to Sunday Surf. This needs to be said… more and louder.
It always makes me sad when I hear people make such statements, especially knowing what I know, I can read between the lines. I wonder if it’s best that they actually believe that, because otherwise, they might be completely frustrated and traumatized…
completely and totally agree! on tuesday may 3rd, i had an unassisted vaginal birth at home after 2 c-sections (UAVBA2C)… by the grace of Allah, all went as smooth as it possibly cud have and both me and my baby girl are doing just fine. my husband and i were forced to take the decision to do an unassisted home birth bc the country where i currently am right now treats it as protocol to do repeat c-sections, and trail of labor is never ever given, infact is considered an illegal practice! i went to so many drs and midwives, but they all refused and said no hospital or poly clinic wud give me a trail at a VBA2C. hence, the unassisted home birth. i wish drs and hospitals become open and willing to accept unconventional practices and not be so rigid and narrow minded in their medical practices!
Pingback: Sunday Surf, May 15 2011: Food, Birth, Early Child Development
Add me to the list of babies who would have died had we been born at home. I was born a few weeks early, nothing major, and I was a good size. However, I wasn’t breathing. I couldn’t breathe on my own for several days, and even in the top notch NICU I was in, I nearly died several times. My parents had to deal with the “if she lives through the next hour, she’ll be okay” speech. It was terrible.
When it was time for me to deliver my baby, there was NO WAY I would do a homebirth. Although I was low-risk and honestly a perfect candidate for homebirthing, I knew that I would not be able to relax, and could see having complications as a result.
In the hospital I had a completely natural hospital birth with few interventions. My OBGYN fully respected my wishes and let me do my own thing. My L&D nurse was amazing and supportive, never once uttered the “e” word and I was only checked twice. Neither pushed me around or held me down. I was allowed to eat, drink, walk around, etc. It was exactly the birth I wanted and my baby was perfect. I obviously could have birthed at home, but I think my own anxiety would have caused a less favorable outcome.
For me, birthing in a hospital allowed me to relax, knowing that if things went south, that NICU was right down the hall. I didn’t worry about me or my baby, and this release of worry allowed me to be totally into my birth, which progressed quickly, easily, and with few interventions.
I had a beautiful home birth, and I hemorrhaged really badly. My midwife was able to stop it & save my life. No hospital. Yet, to this day, I am SO confused as to WHY I hemorrhaged. My birth was totally left alone, very supportive environment. If you have anymore insight on natural home birth hemorrhages, I’d LOVE to hear them. One of the only things I’ve heard so far is that I’m a redhead, and redheads tend to bleed more. That doesn’t settle me enough. 🙂
Loved the Oxytocin hemorrhage poster
Thank you for this article. Great Hemorrhage poster too.
On the BMJ there is a study which actually proves that homebirth are safer than Hospital birth…
Erin,
It is a double-edged sword: Women need their experience of birth validated without the influence of our own political beliefs, AND, as healthcare providers to pregant women we do not want to contribute to the mythology that a woman must be saved during birth because of the political consequences to their range of choices for care.
What is completely missing from the “I would have died at home…” belief is the understanding that women who choose midwifery care during their pregnancy are very closely watched, well examined and carefully listened to during their prenatal care and would be immediately refered to an Ob/Gyn is any signs of risk presented, and would not be birthing at home in the first place.
The either or stance reminds me of the ways we divide women by their choices and call it “Mommy War” instead of listening to each other’s experiences and being curious about what else is possible and how we can improve our range of choices for prenatal and birth care.
Thank you for making time to write. You have obviously provided a platform for a lot of thoughtful discussion.
We planned a home birth for our first son but ended up having him in the hospital when he was born 6 weeks early. I hemorrhaged very badly after he was born. I was encouraged by my OB/GYN not to have our second baby at home due to my high risk of bleeding. He was very adamant, but deep in my heart I knew I had bled the first time partly perhaps because my son was born early and most definitely because it was an extremely rough placental removal (which I didn’t realize until later) with lots of painful stomach massaging and cord pulling. My placenta separated at that point and I lost an amazing amount of blood very, very quickly. Had I been at home and lost that much blood, I probably would have died, BUT I know the situation never would have been dealt with like that. I did have my second baby at home with no complication or bleeding. My mother too hemorrhaged when I was born at home and almost died, but again I knew it was because she was not accompanied by extremely trained midwives who probably could have handled the situation better.
Having been one of those unlucky women to experience PPH, I am beyond disgusted with this complete garbage can of an article. You clearly know nothing about PPH if you think they don’t happen at home. Mine was caused by trauma, specifically a cervical laceration. As soon as the placenta was delivered, I began to bleed heavily. My CNM immediately had the nurse give me a shot of pitocin while she began searching for retained placenta and clots. She quickly ascertained that it was likely a laceration, and sent me to the operating room for repair by a obstetrician. My husband estimates that it was less than 15 minutes from onset to surgery. I lost a lot of blood (had my hematocrit dropped one more point, I would have been transfused). This was after a “textbook” natural birth (no I.V/heplock, intermittent EFM, ate and drank during labor, changed positions for pushing, didn’t push until I felt the urge, delayed cord clamping, immediate contact with my baby, etc.)
I would like Erin to explain to me how she thinks that I would have survived this complication had I given birth at home. No one at the hospital tore my cervix – the act of birth was solely responsible. I live at least 30 minutes away from the hospital. Pitocin and uterine massage were not going to resolve this problem. Please, Erin, convince me that a homebirth wouldn’t have killed me in this situation. How would you feel if I had been in your care, Erin? Would you have had a clue about what to do for me? Please take the time to educate yourself before you go around making grand assumptions about a situation that can kill a new mother within minutes.
I’m just a midwifery student, but I’m assuming the cervical laceration would have been clamped and you would have been transported immediately… A midwife would have likely done the same elimination process of pitocin, searching for retained placental fragments, identifying cervical lac, etc. Is life flight available in your area? Where we practice, we tell moms that if an emergent transport is necessary, they will be life flighted to the nearest hospital.
In your case, obviously, the better place to be was in the hospital- with immediate surgical capabilities, this does not mean however, that a midwife couldn’t have handled this appropriately…
Glad that you are okay.
Have you ever seen a cervical laceration MAP-MT? The blood can come so quickly that you can’t even see where to clamp without appropriate visualization. You need OR suction just to figure out where it is coming from sometimes.
Actually no, but I have been at a birth where there was a cervical laceration. The midwife quickly and calmly clamped it off with forceps… by feel I suppose. Was handled beautifully- no OR needed.
I did recently witness a hospital birth with major lacerations and a retained placenta. Precious minutes were lost as the OB waited for anesthesia. A midwife would have manually removed the placenta and sutured the lacerations- resulting in less blood loss and probably no need for a blood transfusion. P.S. There was suction.
Thank you, MAP-MT for your response. LifeFlight is available, but I question whether the majority of homebirth midwives would have been competent enough to get me that level of care in time. I’m glad that you are working with midwives who understand that PPH can and does happen outside of the hospital setting. I just grow tired of reading uninformed commentary from someone who should know better. I am concerned by the number of HB midwives who encourage high-risk deliveries at home (VBACs, breech, even multiples), and seeing blogs like this make me question whether or not these types of midwives are even competent to attend to low-risk women.
I find it interesting, and a bit ignorant, to group all homebirth midwives into one category.
The majority are extremely well trained, cautious, and knowledgeable.
The majority are also licensed, and required to follow guidelines and protocols set by their state and/or by NARM.
Finally, the majority are NOT cavalier, self-satisfying, pushy professionals who have their own agenda….. No, not licensed midwives; though I can think of one group that embodies those three qualities.
As someone who has worked in the medical field in a third world setting, where women do give birth at home, attended by traditional midwives, with NONE of the interventions you mentioned…..let me tell you: the maternal and neonate mortality is HIGH…..and one of the foremost causes of death is post-partum haemorrhage.
Following your logic: Please explain how this is possible?
I too have worked in an impoverished nation with a high maternal mortality rate and am very familiar with the tragedy of PPH. I never stated postpartum hemorrhage does not happen at home. However, comparing hemorrhage in healthy American women having midwife-attended births at home to impoverished, malnourished women in less economically developed nations is an apples and oranges situation. This piece is about healthy, low-risk American women who do not die from PPH following vaginal birth with any regularity. Published medical evidence shows that 1) use of pitocin in labor increases the risk of PPH and 2) the rate of PPH is lower in planned homebirths of low-risk mothers than it is in comparable births in hospital, and that is what this piece is about.
The women I’ve met were neither malnourished nor were they (by their community standards) “impoverished”. They had houses, kitchens, live-stock and fields and their kids went to school.
Sorry, but just because you live in a third world country, this does NOT mean you’re automatically starving and illness-ridden.
The women were healthy, well-fed, had “normal” pregnacies (the local midwife kept charts and did antepartum and postpartum care too), the birth itself was attended by a local midwife….and STILL they suffered from PPH. Frequently.
Since the women were NOT malnourished, NOT impoverished and NOT otherwise ill, how does this make it an “apple vs. oranges” situation?
Anda, thank you for sharing your experience, but I’m not sure what this disagreement is about? I have never stated that PPH does not occur in all settings.
Typically when the phrase “third world” is used in the context of healthcare and maternity care specifically, it is to infer that women are generally impoverished and lack access to adequate health care providers. If that is not the case with the community you worked in, and all the women were healthy, had normal pregnancies and had access to skilled midwifery care, then yes perhaps they are more similar to low-risk American women birthing at home than not.
Again, healthy, low-risk American women who do not die from PPH following vaginal birth with any regularity. Published medical evidence shows that 1) use of pitocin in labor increases the risk of PPH and 2) the rate of PPH is lower in planned homebirths of low-risk mothers than it is in comparable births in hospital.
The purpose of *this* piece is to highlight the point that events in typical hospital births — and their outcomes — cannot automatically be extrapolated to out-of-hospital settings. I am happy to continue discussing my points in this post in a respectful manner.
Thanks so much for this. I’m currently 30 weeks pregnancy, planning my first homebirth after two very complicated (intervention-based) births. I am so relieved and excited about my natural, normal, birth and reading this just reinforces what I KNOW to be true.
I’m in a similar situation! Saying some prayers for you Mama!
My son was one of those rare babies that actually would have died at home. I birthed intervention-free in a hospital (no IV or hep lock, birthed standing up, pushed with my natural urges, etc) and my son’s cord tore after his head was born. He lost a lot of blood, was white as a sheet, his heart wasn’t beating and his lungs weren’t breathing. Someone yelled that he was a full code and 20+ people rushed in to save him. After 2 minutes they got his heart pumping and they rushed him away and got him intubated.
I guess I felt the need to state that because I hate the look I get from other birthy people when I tell them that my son would have died at home. They immediately assume that I must have had interventions that caused his complication. Heck, I hate the look I get when I say I had a natural birth in the hospital, like I must be confusing “natural” with “vaginal”.
Thank you for your story, M. It is true that “birthy” people, as you say, may tend to assume that interventions led to your son’s difficulty transitioning at birth. They will assume it because, for most low-risk women, it’s true. But there are times when shit happens no matter where you are or who is attending the labor. Even in the very best of circumstances, some babies will not make it. That’s NOT to diminish your story or your emotional experience in any way, I only mean to point to the nature of life, birth. I still believe we can’t look back and assume the same events would have happened at home. In my experience, sometimes babies who need to be born in the hospital find their way there. Not *always,* but often.
I am one of those people who believes she probably would have died at home, but I had grade 4 placenta previa and had 7 APH. My son took 15 minutes to resus after the birth and then spent 1 week in NICU.
I know, however, that we were a rarity and those sort of complications don’t happen to most birthing women. I know most intervention is just to speed things up, it certainly was with my first, induced, epidural, vacuum delivery.
If I were having a third, it would be at home, but my last birthing experience has really put me off it.
I hear that all the time when I talk about my homebirth…sigh…
I came here through a friend’s Facebook post. The article was very informative. And now the obligatory “when-I-gave-birth” story:
When I was pregnant I was under the care of an OB/GYN who had a nurse/midwife who worked in the same office. It wasn’t until it was two weeks past my due date and nothing was happening that he recommended inducing labor. When I got to the hospital that Tuesday night, I was told that it was apparently a very popular night to give birth, and all the nurses were busy — but it seemed that I was having contractions every 7 minutes (though I couldn’t feel them), so they didn’t want to send me home. So I spent the night in the hospital sans any medication. (Fun sidenote: they did have me hooked up to the monitors. I have naturally low blood pressure, and every time I started to go to sleep, my bp dropped enough that an alarm on the monitors would go off and a nurse would rush in to make sure I wasn’t dying. They finally just turned the alarm off.)
The next day they started me on pitocin bright and early. It was about that time that I began to feel the contractions; they felt pretty intense. By 1 p.m. I was tired, and I took a nap. After I woke up, the machine still registered me having contractions with the same spacing (I don’t remember how many minutes between them — 3-4, I think), but I was only feeling one in three. My doctor thought this was odd, so they checked to see how my dilation was progressing. I had started the day at 1 cm; by 5 p.m. I was at. . .1 cm. My doctor told me my options (which were complicated by the fact that his family vacation out of state started the next day): I could continue as I was for another 24 hours or so, and if things went well, I would have the nurse/midwife from his office there to deliver; if things didn’t go well and I needed a c-section, then it would be done by the surgeon on call. I asked him at this point if, in his professional opinion, he thought things would end up in surgery anyway. He hesitated, at which point I said, “I’m not going to sue if you’re wrong.” He then told me that he thought that, yes, I would probably end up on the operating table. I figured if we were going there anyway, I may as well go sooner than later. And so it was that my son was born c-section at 10:19 that night. My doctor later told me that my son’s head hadn’t even entered the birth canal.
I’m no hippie, but I do have a strong dislike for unnecessary medical intervention because I think it’s wasteful and it makes me feel weak. I was the girl who refused to take my percocets after being (literally) hit by a car, because it was unclear at the time exactly what the injury was and I knew if I was doped up it would take longer to figure it out. And though I had a very hard time walking, I was back to work within two weeks. So, on the one hand, making the decision to have a c-section was difficult for me, because it went against everything I had wanted for my birthing experience. On the other hand, I am glad to see articles like this, because you’re right, a lot of that intervention is unnecessary for most women. Giving birth is a scary thing, yes, but our bodies were designed to be able to do it.
I had some PPD, though I refused to admit it at the time, and I think part of it was because being in a position to need a c-section made me feel weak. There was also the c-section related complication of thrush afterward, and after that was cleared up my son refused to drink from anything but a bottle — which was also not at all what I’d wanted. I ended up pumping for two and a half months, and he had a voracious appetite.
I have often wondered if things had been different had I stuck it out. After all, going by the way they calculate due dates, two weeks seems like it’s within the margin of error — perhaps my body just wasn’t ready? But I was also on pitocin for 12 hours with no change in dilation, so maybe my body lost a crucial memo or two. If any of the pros who have commented thusfar have an opinion on the matter, I am all ears. I’m not pregnant now, but my husband and I would like our son to have a sibling or two someday, and I’d like to know as much as I can before then.
Angela, thank you for sharing your story. If you’d like to talk more I am happy to email or chat with you. Here’s my short answer for now: when we force a body and baby that are not ready, to go into labor and be born, the process cannot unfold the same way it would have if it started naturally. Try searching around online for the problems with inductions. Look at the mothering.com birth forum and the ICAN forums. The good news is that if you do give birth again, it is almost guaranteed to be easier and shorter. And next time you’ll have the strength of your instincts behind you, and the confidence to trust them!
The people who rant about dying if they were at home seem to ignore the fact that a) midwives are licensed by medical boards, just like doctors! b) Midwives attend only low risk births c) Midwives do screen for B-Strep, give blood tests, etc. d) Midwives monitor heart rates and many many other signs and transfer at the first signs of problems. e) midwives treat hemmorhage. f) Midwives have a back-up doctor at a near-by hospital. g) Midwives have extensive medical training to care for both mother AND baby. h) Midwives save lives. UNFPA – Executive Director Speaks about the Importance of Midwifery
http://www.unfpa.org
”Midwives are central to the achievement of all three health-related MDGs — 4, 5 and 6–to reduce child mortality, improve maternal health and combat AIDS, tuberculosis and malaria,” said UNFPA’s Executive Director, Babatunde Osotimehin, in a televised message at the launch of the State of World Midw… See http://www.unfpa.org to read the whole article.
Very well-said, Erin! Love how you honor a woman’s perception, yet you still speak truth! Very good reminder. Truth must be spoken.
Thanks for sharing this Erin! I’ve had 3 hospital births, all unnecessary inductions….with the 3rd being the most tramatic. Also causing me to seek out a better way! We’re TTC no. 4 (our last) and planning a home birth. The more I read, the more encouraged I get. I long for this healing birth….and am so looking forward to it.
Brilliant!!!
With my first pregnancy, I was put on bed rest at 24 weeks for PIH and induced 2 weeks early. After 33 hours of no dilation, they did a c-section. That is when they found a baseball size uterine fibroid. I had no idea what a fibroid would cause and the Dr didn’t explain crap to me. I went through my 2nd pregnancy a little over 3 year later wanting a VBAC, maybe even a HBAC. When it came to labor I felt like something was wrong with my contractions. They didn’t feel right and I knew that I would need a c-section. Some of the nurses chalked it up to nerves and some just thought I was chickening out. Once in the OR for the repeat, they found that the fibroid was the size of a grapefruit and half way blocking the cervix. I began hemorrhaging 2 days later and was in and out of the hospital for a month before finally having a hysterectomy. The purpose of this post is to say their are other reasons for PPH. Mine was VERY rare but I do believe that midwife care is the best. I believe in it because I did all the research on VBAC’s and really wished we had that kind of care here. I know that if I was under a midwife’s care I would have been transfered to an OB and probably would have had the same outcome.
This could apply to the opposite ” if I had delivered at the hospital I would have died along with my baby” I am not sure why but the HB community is terrified of doctors and hospital and are just as silly as those people that say that initial quote.There is an amazing amount of fear in the NCB crowd, fear of intervention , fear of drugs, fear of doctors , fear of hospital fear of pretty everything, for a community that proud itself of empowerment there is an awful lot of energy spent perpetrating fear.
There is a lot of fear in our culture around pregnancy, birth, and mothering. That’s for sure. Fear can come from a place of distress, and fear can come from instinct, from our innermost wisdom demanding to be heard. Some fear is healthy, and a vital part of pregnancy and birthing. When a woman’s instincts tell her to be afraid, I believe she ought to listen. That said, birth is also one of those times when we are served by our own detachment and ability to embrace all the possible outcomes.
I find these types of debates exceptionally difficult to read without thinking of a dear little baby who, had he been delivered in hospital, would be alive. We know this based on autopsy results, it’s not just an opinion. My friend who entrusted her pregnancy to the care of midwives and subscribing to the notion that “all will be well because pregnancy is natural” almost died too. I can only thank our emergency services who talked her partner through reviving her whilst the midwives tried to revive her son. I know you talk about “low-risk” and I agree that many women have had wonderful birthing experiences at home and I will support their choice to do so. My friend however was supported by a group of midwives to have no obstetric care and a home birth despite being 38 yrs old, first pregnancy and obese. I do not regret my decision to have two elective caesars and am eternally greatful that I have two healthy children. I’m also thankful that my friend now has a beautiful daughter, born via elective caesarian in hospital. No doubt I’ll be considered simplistic saying this but at the end of the day let’s just stop the debate and accept there are multiple ways in which babies enter the world – if they are born healthy and alive, who cares how they get here.
Melinda, I can’t speak to your friend’s experience because I do not know anything about her, her labor or birth, or midwives. I believe how babies enter this world is extremely important to mothers and babies alike. Millions of other women believe so too, and that is why the birth change movement in this country has arisen from birthing women themselves, and has transformed the lives and experiences of countless women. I understand if the manner in which you birthed your babies, and the way your children entered this world is insignificant to you so long as they were “healthy.” But how we birth babies IS a big deal to many women. We can certainly honor that while respecting our different experiences, no?
I really love this!… until the last line. It really frustrates me how the midwife community has taken on this concept of risk status when it comes to birth. If we truly believe that birth is a natural physiological and involuntary process (meaning the body knows how, when, and why do to it) and that it has been medicalized, how can we build our paradigm of safety on the medical model which views the female body as abnormal, and the birth process as a medical procedure.
Medicalize : to view or treat as a medical concern, problem, or disorder. “Medicalization is the process whereby normal functions of the body come to be seen as indicative of disease”
Birth has been medicalized, and midwifery is more and more taking on that medicalization and owning as its own paradigm. It’s very difficult to escape the medical thinking that has us comparing home to hospital as the gold standard and talking about risk as if pregnant women are problems waiting to happen, but some women, low-risk women, are healthy enough to attempt this procedure without the safety of medical care.
I’ve come to really hate that term “low-risk.” It’s a cop-out; it’s a way to claim birth is normal but imply at every turn that birth really is risky. It’s a way for the medical model to keep its strangle hold on women’s birthing, and use midwives to do it. And it is the medical community who defines that risk, not the mothers who rightfully own birth and must ultimately accept any inherent risk in childbearing, or the midwives who are increasingly enforcing the construct of risk in home births.
If we really want to be free from birth medicalization, we have to build our paradigms on a new foundation of trust and reject all forms of medicalization including assessment and assignment of risk status.
I am the “crazy” lady on the other side of this fence.
I truly believe that if I had not been with a midwife for my 2nd and 3rd pregnancies the outcome would have been a lot worse.
My second needed resuscitation when he was born, but they left the umbilical cord attach to him the entire time they were doing it so he was still getting the oxygen rich blood through it to him. The would have clamped that cord almost immediately had we been in a hospital and I really think his brain would have suffered from that.
With my third son I was showing signs of pre-eclampsia and instead of wanting to set up an induction like my ob with my first son did, my midwife had me increase my protein and start drinking lots of dandelion tea. That made it possible for me to have my son show up on his own time schedule.
Wow, what a great post! I am newly-married and definitely thinking about how I want my future children to be born. I’m thinking about a home birth and I’m wondering: What qualifies a woman as “low risk”…and what qualifies “high risk”. I have underactive thyroid, but am on a very low dosage. Wondering if this would affect the risk level at all.
Thank you for writing this ❤ Lots of love, from a doula, who birthed her own baby at home.
I’m a little late 🙂 But I wanted to add that in my case, I had scar tissue on my uterus from a termination when I was in my teens. The placenta adhered to this tissue (which was in a concave area on my uterus, so the wall felt flat and normal), and caused a post partum hemorrhage. I had to have 8 bags of blood, around 5 litres. I live in a rural area, and a transfer would have taken me only to the nearest hpspital (where I actualyl birthed), which had 2 bags of my blood type on standby. I had to be transferred by plane to the nearest metro hospital. If I had birthed at home, the extra time needed for the transfer may well have meant that I died.
It was a hemorrhage factor independent of the pitocin/oxytocin dynamic – completely caused by placental adhesion to scar tissue.
And while I certainly believe women should be allowed to birth at home if they want to, I would like to be able to tell my story without people immediately sitting back and tsk-tsking me either!
I’m late, too, but this needs to be said..
I might have been OK having a home birth. My baby would have been in danger. I am healthy, under 35 and had NO risk factors AT ALL for premature placental aging (verified postpartum by the hospital pathology lab) and a placental abruption. No warning signs, no nothing. I had a 36 week checkup and everything was normal, a little effacement, certainly no signs of imminent labor. 24 hours later I was in true labor, bleeding profusely, and 4 hours after that my child was born, blue and floppy, with lungs full of aspirated blood. The only reason I didn’t have a c-section was that he came out too fast. I can’t even describe what it feels like to hear “get the respiratory team in here” and have your tiny newborn pulled away as soon as the cord is cut, then whisked out of the room (he was fine after suctioning and a few hours of oxygen and monitoring, fortunately). As for me, I was pretty happy to have IV fluids and pain medication after losing that much blood, not to mention vomiting all through labor.
I wanted a natural birth. It didn’t happen. After processing it for several months, intensely, I am left with gratitude for the nurses and doctors who helped my child breathe. No blame, no regrets. And if I had told someone about that and they’d rolled their eyes and said “mmhmmmm” ..I can’t even imagine what I would have done.
Don’t tell other people what happened at their birth. Let them tell you. Then judge, if you must.
Comments like this have been confusing me, and I mean no disrespect at all in saying that. I just don’t understand what a very unique experience like this has to do with homebirth. If you were under a midwife’s care at home when you started bleeding, you would have gone to the hospital just like you did anyway. Midwives don’t lock the doors and keep women from the hospital when transfer is needed, they are absolutely your diligent caretaker in observation and action.
I have 2 friends who have suffered placental abruption in homebirth and both times their midwives saved their baby’s lives by ensuring EMTs didn’t force the mother to lay on her back during transport as they are taught to do and instead supported the mothers in transport on all fours.
I get that birth can be unpredicatable and downright scary, but this stuff happens no matter where you choose to give birth. Saying that your baby almost died is a true statement, but being at home BEFORE a complication and within reasonable transport distance is logical and safe in low-risk pregnancy and birth. The odds of something like placental abruption is like 1%, which is similar to the risk of pitocin-induced uterine rupture and yet you hear very few women say “My baby would have died in the hospital” despite pitocin induced labors being the absolute norm in that setting.
I don’t want to offend, I just feel like this argument against homebirth for inexplicable circumstance are not at all what is being referenced when the topic of the safety of homebirth is being discussed yet it’s brought up again and again.
Any eye-rolling I’ve seen has been in reference to the majority of women who say “My baby would have died because of my blood pressure crash (epidural), emergency c-section (epidural), vacuum extraction (epidural), etc.” Not to say this is ALL cases, of COURSE, but I’d say that OBs are very skilled at leading their patients to believe that these interventions were necessary to save the baby and that they are never willing to admit that their “safe” interventions played the most important role in the decline of the mother or infant’s health.
There are exceptions to every rule, but in the case of birth, those exceptions are very rare.
A, thank you for sharing your story. While I can’t comment on the clinical aspects of your birth, it sounds like it was terrifying and I can only imagine how that was for you. I do not believe, however, that I “tell other people what happened at their birth.” I offer one counter perspective here to the inflammatory statements around birth place. I am only human! I have my faults. This piece, and the part about me listening to women’s birth stories, is an honest testament to that. I am not free from judgment by any stretch of the imagination, and I am not immune to settling in to my beliefs about birth and interventions, but I certainly DO strive to listen to every woman’s story with love and kindness.
I agree that we shouldn’t jump to conclusions based on what we read on the internet. That includes not jumping to the conclusion that the baby or mama would indeed have died or that the midwives/doctors were at fault etc. based on the moms account of labor. While I don’t think that moms lie about their births, I do think that sometimes details get jumbled up or misunderstood. I have seen personally how the account of the mother can vary drastically from the account of the labor record or the midwives present. It is a good lesson for us all to take everything we read with a grain of salt, and not jump to conclusions being that we weren’t there.
On an unrelated note, so many times i hear in the accounts of women who feel their babies were born very compromised, that their baby was born blue. I have to point out that blue or purple is a normal color for a baby to be born. Being born pale or white is a much bigger problem.
It is a valid point that a lot of emergencies are caused or worsened by hospital policies and procedures, including interventions. Not disputing that at all. When choosing home or hospital birth, people choose which set of risks they are comfortable with and I totally believe in the right to choose.
Maybe you’re right that I would have been transferred. I don’t know if a midwife would have transferred me; I’ve never seen one or asked. Some bleeding during birth is normal, it’s a judgment call as to how much is too much. But I see your point. My point is that it’s unfair to mothers to automatically assume their story is invalid.. especially before it’s even really heard. I’m not saying “homebirth is unsafe because x y z can happen,” I am saying, “please don’t assume that the mother doesn’t know what she is talking about.” Having a birth that was not what you planned for and was scary and traumatic is very upsetting. Having someone minimize or invalidate that is painful.
Being born blue, to my knowledge, is not ideal. My child got an apgar of 4 because he had a pulse. He wasn’t breathing well, moving well, or responding well.
I love to share the story how my baby would have been in the NICU if I had a hospital birth. Instead I had a very patient midwife, who, when my labor stalled at 36 weeks, sent me home. I carried that baby for five more weeks and she wasn’t even 7 lbs at birth. In my first go at labor, I had dilated to a 7 before it stalled and then I went back to a 3! At a hospital, my water would have been broken and I would have given birth to a very tiny 36 weeker. Hospital birth is not all that it’s cracked up to be :)…………….I was birthing at a freestanding birth center 🙂
Thank you so much for explaining these differences with so much love. I’ve been fighting with our helth care system (I live in Montreal) for the past 3 weeks to have an at home birth. Trying to explain to everyone that I am safer at home than in a hospital. This is my third and probably last child. I really hope I can offer her that gift.
The NC woman you mention at the beginning of this post is a family friend, and actually delivered my brother (who is now 18). The local news certainly took their liberty in telling the story. I had to stop watching as there were so many incorrect statements in their reporting.
My desire was to have homebirths, but my husband was hesitant, so we delivered both times at the hospital…intervention free. We had a great experience both times, but I contribute that to the fact that the nurse we had for both births had been a Doula & was a great advocate for what she knew I wanted.
Perhaps my husband will agree to a homebirth next time around 🙂
“The CDC has estimated that half of maternal deaths are preventable.”
Exactly!
You forget to mention that the CDC says (capitals mine, of course), “Nevertheless, more than half of all maternal deaths can be prevented through early diagnosis and APPROPRIATE MEDICAL CARE of pregnancy complications (6,7). Hemorrhage, pregnancy-induced hypertension, infection, and ectopic pregnancy continue to account for most (59%) maternal deaths.”
Now, here is my speculation (at least I’ll admit to it): homebirth only worsens maternal death rates. CPMs don’t have the tools or knowledge to detect or prevent these problems and often play down their importance. The newest phrase in homebirth will probably soon be the “dead mama” card.
Yes, the primary causes of maternal mortality in the US do not include hemorrhage at planned homebirths. Women are not dying from hemorrhage at homebirths in the US. We all want the maternal mortality rate to shrink, that is a shared hope and goal, correct? As the only maternity care providers trained to practice specifically in the homebirth setting, CPMs are an important part of ensuring the safety of mothers and babies in planned homebirths. Published evidence from medical studies on homebirth in the US, Canada, UK, and Netherlands shows a 0% rate of maternal death from hemorrhage at home. if you are unfamiliar with the training and educational requirements for CPMs, that information can be found here : http://narm.org/
You’ve failed to include the other risk factors for uterine atony, focusing solely on Pitocin. If one did not know any better, one might assume that there are not many other risk factors. Pitocin augmentation is one of 14 possible factors.
Table 1 Risk Factors for Uterine Atony
Factors associated with uterine overdistension
● Multiple pregnancy
● Polyhydramnios
● Fetal macrosomia
Labor-related factors
● Induction of labor
● Prolonged labor
● Precipitate labor
● Oxytocin augmentation
● Manual removal of placenta
Use of uterine relaxants
● Deep anesthesia (especially halogenated anesthetic
agents)
● Magnesium sulfate
Intrinsic factors
● Previous postpartum hemorrhage
● Antepartum hemorrhage (placental abruption or previa)
● Obesity
● Age > 35 years
Seminars in Perinatalogy. (2009). 33(2):82-7.
Thank you for your comments. That’s right, I use pitocin augmentation as one example of why birth events and outcomes in a hospital setting cannot automatically be extrapolated to homebirths. (We don’t augment labor at home with pitocin or any other medication). While I do indicate that hemorrhage can and does happen in any setting, the purpose of this piece is not to outline the causes of maternal hemorrhage. But to be clear, READERS: there are many causes of hemorrhage, some of which are listed above.
My parents raised me to understand that every medical intervention comes with the possibility of a complication. As an adult I have always been wary of medical interventions and I’ve also been fortunate to be very healthy. I got to my late 30s never having had a surgery, or a blood transfusion, never having been an inpatient in a hospital, taking no regular medications.
So of course when I got pregnant I chose a very good practice of midwives. They are very experienced and very competent, and I looked forward to a natural childbirth. Then I got sicker than I have every been in my life. I developed severe pre-e with high liver enzymes and low platelets. Even as I got sicker and sicker between 27w and 29w, my body showed absolutely no sign of going into labor. Thankfully the system worked as it should. My midwives recognized my serious symptoms and sent me to to the hospital. I survived a birth that made everyone involved pretty nervous and my little baby did well in the NICU.
I think the basic premise of this piece is a good one, all women (all people seeking any kind of health care) should be aware that the cure can be worse than the disease. However, I am deeply troubled by your lack of respect for those of us who risk our lives to bring our babies into the world. Several times in this piece you reference the difference between what you say to a woman who tell you that “I would have died” and what you are actually thinking. While you don’t directly tell us your internal script, I imagine it runs something like this “you poor thing, you were duped by the medical establishment. You are kind of a drama queen.” The only cure for my condition was delivering my baby, but my body would not let her go. Without an induction or a c-section (services available in hospitals) I would have developed uncontrollable eclamptic seizures. When you listen politely to women like me are you thinking dismissive thoughts (I guess you didn’t take very good care of yourself, well I guess you should have been in the hospital, but you should tell such a negative birth story to impressionable pregnant ladies)?
Those of us who could have died due to pregnancy or birth are women. Our experiences are human experiences. We should be respected as the survivors that we are. Our experiences should remind anyone who cares about women that mothers in Afganistan, Congo, Sierra Leone, etc. are dying everyday because they don’t have access to quality health care.
I really don’t understand why acknowledging us without dismissing us or tearing us down feels so dangerous to people committed to natural birth.
I still believe in natural birth, so it’s hard to accept that natural birthers don’t believe in me.
I had a delayed postpartum hemorrhage at home with my third. My midwife was back at my house in a heartbeat, and we dealt with it at home. I share my story as often as I can, because everyone asks, when they hear a friend will be birthing at home, “What if something goes wrong? What if she has a hemorrhage?” There are so many skilled midwives out there, who are in general m
My sister and another friend both fall into the category of “I may have died if I had a homebirth.” They had spontaneous placental abruptions, neither of which was caused by any medial interventions. My sister lived 45 minutes from the nearest delivering hospital and happened to be in town when her contractions began. They had 6 minutes to deliver my niece before the lack of oxygen would have damaged her, she was out in 3. I see Divine Intervention as the reason her birth was successful.
My other friend had her water break at 34 weeks at home, blood soon followed… her baby girl was delivered via c-section at her hospital, where she had been planning to have a natural vaginal delivery with a supportive OB/Gyn all along.
In both cases,. to my knowledge, the presence of the needed medical care saved their lives.
I personally will never be able to relax enough at home for a productive labor, well unless this baby comes so fast I can’t get to the hospital. My son was born naturally at 40 weeks 6 days in a hospital under supportive care. Did it have the personal touch of midwifery? No. But when I went in for my 40 week check up, the doctor on the team who I had least expected to be supportive said she would not rupture my membranes because I was progressing well and she was confident my son would come in his own time before 42 weeks.
I have yet to hear how my sister or friend’s lives or at least their babies’ would have been saved given their rare yet significant situations….
I appreciate the article, but it does not offer any insight into the situations I have observed, just those in which interventions may have caused the problems.
Lauren, those are scary situations you’ve described. I think regardless of their intended place of birth the hospital was ultimately a life-saving factor. I don’t believe the author is arguing these types of scenarios.
On the other hand, worth mentioning here is that even when a woman has supportive care with a doctor, it is not the same level of care one would experience with a homebirth midwife. In the latter setting, a mother would receive 1 hour prenatals (time spent with the midwife, not waiting for her). During this time, the midwife is not only forming a relationship with mom, but also continually looking for early signs of such complications or risk factors that would preclude her from remaining a good candidate for homebirth. Much of her care involves education and support in areas that help maintain that mom remains in a low-risk category, including ongoing conversations about her nutrition and lifestyle. Many predisposing factors for pregnancy complications include lifestyle choices.
That said, sometimes true emergencies do arise. They arise in any setting, for a variety of reasons. A homebirth midwife is trained to pinpoint signs of potential complications and act accordingly – sometimes this involves transferring care in pregnancy or labor. I’m certain that even if the two women in your stories were planning a homebirth, the outcome would have been the same. Both situations are outside of a homebirth midwife’s scope of care and she would have transferred care, accordingly.
I’m so glad to hear that these births had positive outcomes. These are the kinds of situations that we can be so grateful for medical intervention.
Very good point.. I can’t help but wonder what may have been missed, in both cases the pregnancies appeared picture-perfect. I wish there were more hospital based midwives and birth centers available because it really would be nice to have more personal attention during visits than the norm for those of us who can’t get past that “what if?”
So true. I got one of the “my baby wouldn’t have made it if I were at home” comments a couple of weeks ago. (The mother was diagnosed with CPD and had a cesarean.) I felt myself burning inside, thinking of all the different reasons a baby might not be coming down through a pelvis besides true CPD. I thought to myself, “I wouldn’t have had a vaginal birth if I were in the hospital!” (I’m quite certain of this- I pushed for 3.5 hrs-posterior baby- before he finally made it under the pubic bone and came out. I probably would have been diagnosed with CPD too.) I know I’m rambling a bit, but the point is that I am thankful for your post. It is difficult to be quietly understanding without raging about all the misinformation out there! I am glad to read a post from someone who feels similarly. I think knowing when to dispel the myths and when to listen empathetically is probably one of my greatest challenges as a doula.
Reblogged this on the birth bug and commented:
I recently heard one of these statements myself: “If I were at home, my baby wouldn’t have made it.” While tragic outcomes can happen in any location, it is important to remember that one cannot extrapolate hospital events to home birth situations, nor home to hospital. The environments and practices of caregivers are far too different to make a judgement call as to whether or not you and your baby would have survived elsewhere.
I find that one of the most difficult challenges as a doula is knowing when to dispel the myriad of birth myths floating around, and when to quietly listen to a mother’s story without speaking up. There is a time and place for everything, and I am working on knowing the right times for each role. Any suggestions, anyone? Please read the whole post over at erinmidwife.com
so glad you are taking on this topic, with courage, heart and rational thought.
These fears need to be dealt with so change can happen.
Reblogged this on Jmportraits's Blog and commented:
Love this, hello world!
I think the premise of this story was phrased very well. I am due for my second attempt at homebirth in August. The first time I did have to transfer to the hospital but I blame the establishment for that and I really appreciate the care my midwives gave me at home and once I got to the hospital.
The story: I had been diagnosed with gestational diabetes but I didn’t agree that I actually had it. My sugar levels were controlled just fine with my diet but my doctor was still worried that my baby was going to be too big and refused to let me go until full term. So with the expert care of my midwives, we worked for a week to induce labor at home. Once we finally got the contractions to stick, I was already exhausted from days of castor oil, excessive exercise, etc. After two days of heavy labor at home with little progress, we made the decision to transfer to the hospital.
I knew things were going to be more stressful and different there but I stuck to my guns and had a supportive husband and midwifery team to back me up. My doctor immediately started me on pitocin and antibiotics (since my water had been broken for over 12 hours). After 12 hours of pitocin and 4-minute contractions back to back, I was still only 8cm and my doctor told me that I needed a C-section. So when they gave me an epidural in preparation for the C-section, I dialated fully and was allowed to push since my baby’s heartbeat was still strong. 30 minutes later, I gave birth to a tiny 7-pound even girl.
I will not be inducing this time no matter how “big” the doctor thinks my baby is getting. It was that poor and inaccurate “diagnosis” that started the cascade that led to me in the hospital with an epidural that I didn’t want.
In conclusion, I still had to pay the midwife (which was understandable) and got stuck with a $10,000 hospital bill that went to creditors and ruined my perfect credit thanks to the incompetency of the hospital billing department. My daughter got poked and prodded unnecessarily because of my “gestational diabetes”. She also was sluggish for over a month because of the epidural. I just hope there won’t be any long term effects on her except the scar on her foot from where the hospital staff drew blood so many times.
I also think it’s so important that we don’t make doctors out to seem like monsters. I should go to Vegas because I’m part of the 1% who suffer from hyperemesis gravidarum and part of the 10% or less who had post-partum hemorrhage and YES, I had a natural childbirth. But during my HG, I was hospitalized several times from dehydration, also malnourished, and that’s where I met my doctor. My doctor was very natural and has even written books about natural approaches while speaking against unnecessary c-sections. He visited with me for well over a half hour to an hour every time I saw him and because of my condition, that was ONCE A WEEK! He didn’t take on so many patients so that he could do this. With my second baby, I birthed in a hospital being able to walk, squat, sway, using my breathing and concentrating on my body opening up. I didn’t even have an IV (trust me, I was sick of IVs). When I became further along in my labor, I sat in an indian style position with the bed in an upright position. I pushed in a sitting/squatting position. My baby was immediately put on my bare chest for the whole duration of the delivery of the placenta. Then I began to hemorrhage. It was even more painful than labor, but I applied the same breathing methods and concentration while my doctor reached up inside and massaged my uterus with his hands. Again, I didn’t have an IV so there was no medicine intervention until a few minutes later when my heart rate was 180, my blood pressure was 110/40, I begin to see black spots and was really out of it, I was then given shots into my thigh. The whole time, the doctor massaged my uterus and got the bleeding to stop. Whereas I know a midwife is perfectly capable of doing this and would do this, my doctor took these measures rather than something more drastic. Anyway…I just find it disheartening that there is a biased opinion toward doctors just as there are a biased decision toward midwifery. There ARE those few doctors out there who are perfectly fine with and advocate the natural birth experience. I’m currently 7weeks and 3 days with my third and currently going through HG and yes, I have the same doctor! It took me everything I’ve got to type this right now because of how sick I am. But I just love my doctor and wanted to voice this.
Natalie, I’m so glad you had the experience with the doctor that you did! He sounds like a gem. I can speak for myself, and I think for birth activists in general, when I say that I / we are not opposed to all doctors but to institutionalized birth as a whole. That means that I am opposed to the system and recognize that there are those who choose to operate outside of those parameters. In fact, as a childbirth educator and doula, I have been known in the past to refer my hospital birthing clients to a certain doctor over a hospital midwifery practice because this doctor held more strongly and consistently to a midwifery model of care than the hospital midwives did.
Congrats on your pregnancy! HG certainly requires medical help. Hugs and blessings to you as your prepare for your upcoming birth.
P.S. My doctor discussed with me that, in theory, I could have hemorrhaged because of the traumatic vomiting I had throughout my pregnancy and wasn’t as healthy as I could have been. I’m embarrassed to suffer from this condition because I am such a natural advocate is so many areas of my life. However, HG is one of those things that I absolutely have to have medical help with. For myself and my baby.
continuing..so someimes us women are aooo caught up in labor i believe i wasnt thinking clearly..i REALLY NEEDED AN EXTRA BOOST OF WOMEN POWER..instead my dr.said..well we can speed things along and give you a minimal amount of Pitocin drip and an epidural…you will also need an IV because you wont be able to drink any fluids..and you will need a catheter to drain your bladder…UGH UGH UGH !!!!! and here i said before huh??? i am low risk..very healthy..exercised all pregnancy 1 hr/day ate many many steamed veggies and lean protein…and am 36 first preg…i have not ever had a headache in 20 yrs..no broken bones..i do NOT even take Advil or aspirin if i have an ache or pain..i just say..hmm its my bodys way of talking with me to back off……sooo know ugh…i had not seen a dr. for an entire decade before i got pregnant..and know i was seeing a dr. every week!! UGH …and NOW…THEOSE DR.s want to do all these invasive procedurea!!! Ugh!! Well i was not feeling the best..with all that pain ina the rectum area..well hmm i said i just felt like giving up…well by 14hrs after i arrived at hospital they had Me hooked up to IV and Pitocin and epidural and catheter…well 23hrs after arriving at hospita (9hrs after Pit+Epi)…i was informed we were @ 10cm ..and i could push…well 3 pushes and 20min later we hd a Baby boy in our arms….I was smiling…extremely hot very flushed..the nurses opened windows temp was 8 degrees outside…i was a bit low feeling..as i was thinking..huh.. wasnt i supposed to feel a ggreat fantastic rush of hormones?? wasnt i supposed to be crying tears of joy?? instead it felt weirdly disjointed…and unconnected..i smiled a rather forced smile…dr.yanked on umbilical cord with cord she wrapped arount a pair if hemastats..and yanked placeta out.hmmm that not what i remember discussing.. . beautiful boy…healthy 6# 9oz….. 41 weeks… Hospital birth…. 180 degree opposite of what i had set out to accomplish in terms of labor and delivery. We are still grateful there was no C section!! AND WE ARE GRATEFUL HE US HEALTHY! thanks for reading!!
Thanks for this post! The truth is that comparing hospital and home births is like comparing apples and oranges. They are two entirely different things. What I find most challenging as a natural birth advocate is our national desire to pretend like every single bad outcome could be prevented. No matter where a woman gives birth, there is a tiny chance that her baby could die or have trouble and there is an even tinier chance that she could die or have serious health consequences. There are risks to giving birth. Our culture simultaneously denies that these risks are real and exaggerates them. That is a crazy-making combination for pregnant women! I’ve come around to understanding that wherever a woman feels safe, she is most likely to produce the best hormones for a good birth experience. Messing with a woman’s sense of safety can lead to real problems in labor! As an anthropologist, I have interviewed hundreds of women about their natural births in and outside of hospitals. I find that if a woman chooses to give birth in a hospital, she often cites “safety” as one of her top reasons for her choice. Ironically, I find that if a woman chooses to give birth outside of a hospital, she often cites” safety” as one of her top reasons for her choice. Even more ironically, all these women are right. 🙂
My birth stories are probably not unique. I became quite ill with pre-eclampsia at 38 weeks with my first daughter…and I truly believe that this was due to a complete absence of education regarding nutrition during my pregnancy. I ate whatever I wanted, and carted TUMS with me everywhere I went due to severe heartburn. Swelling started at 24 weeks. Proteinuria started at 34 weeks. 27 hours of labor, BP’s 170/110’s. I barely avoided a surgical birth. My daughter was kept in nursery jail for suspected seizures (I was an L&D nurse at the time….no way was she seizing. NO WAY). The worst possible breastfeeding “support” leading to jaundice. Suspected mastitis (it wasn’t), for which I was advised to apply cold compresses and avoid nursing on that breast….the exact opposite of what any OB/peds provider should advise. This was under the care of the best CNMs in town.
Second pregnancy: I really wanted a water birth. Sought the care of the best LM in the area, who was known as “the nutrition nazi” in our state! Still had a little swelling and slightly elevated BP at term, but nothing like my first. She spent hours educating me about better food choices and natural options for my reflux (ended up using homeopathic Capsicum with great success). Wonderful home water birth of my beautiful daughter with her little hand on her head. Then….placenta with a large piece of retained membranes. Lots of education about what to watch for, daily PP visits for 5 days, and it passed uneventfully. I we’d been in the hospital, I am quite sure I would have been whisked to the OR for an unnecessary D&C.
Third birth: Nuchal cord and shoulder dystocia. Handled brilliantly at home in water with an LM. In a hospital, would have likely had cord clamped and cut before the shoulder dystocia had been found, and a tragic outcome might have occurred.
My worst outcome was in a hospital, and by the Grace of God, I avoided a c-section, severe over-medication of my healthy daughter, and the loss of my milk supply. Could have been so much worse. My best outcomes, with several potential complications, were with skilled home birth attendants.
Please correct me if I’m wrong, but your first birth, which seems to have had so many complications, was “under the care of the best CNMs in town.” Why then are you blaming the hospital folk? Per this article, are midwives not the anti-hospital folk? If would seem that your worst experience was with the non-hospital, midwives.
Also, please don’t assume that the shoulder dystocia of your third birth would have been missed in the hospital. Even the most green of interns is trained and well educated to NOT MISS shoulder dystocia. Maybe you did not actually mean that the dystocia would have been missed but rather simply that the cord would have been cut before the dystocia was noticed. To this, I would just like to say that the cord cannot be cut until the baby is out enough for the cord to be visible…if you have a shoulder dystocia, enough of the baby cannot be out for you to be able to reach the cord until you have reduced the dystocia (think about it, if the shoulder is stuck, how could the UMBILICAL cord ever be visible? The shoulders come waaay before the abdomen of the baby.) By the time the cord is ever even available to be cut, you have noticed AND successfully taken care of a shoulder dystocia. It is physically impossible to do what you are suggesting…cutting the cord before noticing that there is a dystocia.
“Please correct me if I’m wrong, but your first birth, which seems to have had so many complications, was “under the care of the best CNMs in town.” Why then are you blaming the hospital folk? Per this article, are midwives not the anti-hospital folk? If would seem that your worst experience was with the non-hospital, midwives.”
Really? The CNMs were within a large OB practice, where they only attended births in a hospital. Are you a little stuck on the generalization of the term “midwives?” It seems apparent to me that the vast majority of folks who know anything about home birth realize there are at least two categories of midwives. CNMs can attend home births in some states, but are more likely to practice in birth centers or hospitals. CPMs, LMs and DEMs are more likely to attend home births. Perhaps that clarification will help you interpret the alphabet soup.
“Even the most green of interns is trained and well educated to NOT MISS shoulder dystocia.”
I agree, but I submit to you that the vast majority of SD are CAUSED by provider actions. As a nurse, and a young LM, I saw the same scenerio over and over, hundreds of times: once the head is birthed, it is a complete state of panic to get that anterior shoulder delivered. Yanking on the head ridiculously. Once I learned to wait until the next contraction, IF the head remained a healthy , pink-perfusion color, the shoulder will almost always appear spontaneously. Even on the biggest of babies. I’ve had the pleasure of attending many births of 10+ lb babies without real challenges. I know a day will come when this will not work, but as yet ~
And when I say that my son’s head birthed, and turtled, and darkened, and a nuchal loop of cord reduced, I guess you will just have to trust me. I understand what you are saying, but I have seen one nuchal cord cut with a severe SD by an OB in a hospital, and have read about others. Purple-black head, tight cord (or an occult loop which could not be reduced….it was a while ago and I can’t recall exactly) that was cut, and multiple maneuvers used to deliver the baby. Female OB wrenched on the head, with a leg lifted and foot used against the bottom of the bed, so hard…it was horrifying. Baby left our facility seizing. Perhaps you haven’t seen it, but I have ~
It seems clear to me that her first birth and what she described as her ‘worst outcome’ was in hospital attended by CNMs, but let’s let Momandmidwife clarify.
“Maybe you did not actually mean that the dystocia would have been missed but rather simply that the cord would have been cut before the dystocia was noticed.”
Yes, that is almost exactly what Momandmidwife wrote. She states was an L + D nurse; I doubt she is unclear on the physiology of SD.
Oh, I see you’ve already replied. Allrighty!
I am a little concerned that the overtones of this article and all the comments seem to be the following: “Midwives champion homebirths, and doctors are the ones who do hospital births.” Lots of midwives deliver babies in hospitals. The midwives in our practice deliver babies in the hospital. It is definitely not so cut and dry to just say, “Midwives do homebirths.”
Unfortunately, the availability of certified midwives in hospitals is very limited in some areas of the country. Many (perhaps most) OB/Gyn practices or delivery wards here in TN do not have midwives at all. So here, if you have a midwife assisted birth it is usually at home or one of the very few birth centers that truly encourages natural childbirth.
I wish I had the option to do home births for women at this stage working in a hospital is my only option and I hate it we are undermined and very rarely get left alone with a well normal woman without a doctors trying to get there paws in the woman and usually screwing up the process in someway
AMEN! I know exactly what you are talking about. I hear that all the time from people who hear that I have my babies in a birthing center!
As a midwife working in a hospital I understand the need for doctors operating rooms and cesareans and yes some women were in the right place to have there baby as they may have well died at home in the same situation, these women also tend to be ignorant to the process of labour and birth and totally disconnected from there bodies and so out of tune with its natural process that its a miracle anything even happens and that they both survive. This is our problem with society some women simply don’t care to be informed and educated for whatever reason and are leaving it all up to the doctors. In these cases I rarely feel sorry for the poor outcome, we all need to take some own us on the situation and empower ourselves, if we do not how do we expect a good outcome, we may both survive but at what cost?!?
On the other hand a totally informed spiritual person in tune with her body and senses knows that going to a hospital to birth is not needed she has equipped herself mentally and physically with all the tools she will need to have a wonderful successful birth at home where she feels safe and has chosen who will be there. This is what birth is about we all need to wake up and put more thought into our choices and actions and make a difference for the next generation
This is definitely a charged discussion. I agree that women need to be more well informed of the options available to them, the birth process itself, and the cost/benefit analysis of both birthing at home and in a hospital setting. My desire was for an unmedicated birth in a hospital setting, possibly with a doula or midwife (this was available in my area). However, due to quickly becoming a high-risk pregnancy (sub-chronic hemmorage, low papp-a, pre-e, placenta previa), I didn’t even have a chance to pursue this route. So I had a c-section without ever having to labor. I am glad I knew ahead of time so that I could get used to the idea. The one thing that makes me very grateful in hindsight for the c-section, is my last pregnancy complication, which no one saw, because there isn’t always a way to see it: placenta acreta. Already having a c-section made what could have been a traumatic birth experience, not to traumatic. There was not rushing to a hospital from home or to the OR from an L&D room. I could have had a low-risk pregnancy and still had this happen.
All that being said, I am a huge advocate of the less intervention the better. I hope that one day that hospitals will be more accomodating of this without the Mom and Dad feeling that they have to fight for it.
While I am an advocate of low intervention when possible, I also feel that these discussions are so one-sided. I feel a twinge of guilt when reading articles like this or talking to people who are proponents of homebirths because I feel that they spend so much time expousing the benefits of the homebirth to the point where it makes those who either chose the hospital or did not have a choice feel like they are bad mothers that didn’t do the very best thing for their baby. I didn’t get the skin to skin time, I didn’t get a chance to breastfeed my baby within the first hour, I didn’t get a chance to even try a natural childbirth, all which was best for my baby. Part of this was due to my complications during the c-section and being in the OR longer than normal, part was due to the hospital. I feel like discussions in the article are very one-sided and at the very end are like, oh yeah, this is only for low-risk patients. And yet, you aren’t even willing to define what that means.
I see this same issue with breastfeeding too. Despite some women’s best efforts, they can’t breastfeed. I know women who have been to lacation consultant after lacation consultant, used an SNS 10 times a day and pumped 10 times a day, etc, and still did not produce enough milk. There can be physical reasons why this happens, yet the LC’s just put them down for not trying hard enough and made them feel horrible. The next thing they knew, they missed their babies being babies. They didn’t bond with them because they were so focused on doing ‘the best thing for their babies’ that in the end, the didn’t do the best thing for their babies. This side of the coin is never discussed and I feel that for both breastfeeding and homebirthing it victimizes some women who don’t have this choice, but are led to beleive that they do because these issues are not discussed.
Please educate women, but give both sides of the story.